Vitamin D & Statin Tolerance Checker
Vitamin D & Statin Tolerance Assessment
For millions of people taking statins to lower cholesterol and prevent heart attacks, muscle pain isn’t just an annoyance-it’s a dealbreaker. About 7 to 29% of patients stop taking their statins because of muscle aches, weakness, or cramps. And for years, doctors have wondered: could low vitamin D be making this worse?
The idea sounds simple. If you’re low on vitamin D, your muscles might be weaker. Statins can also hurt muscles. So maybe fixing your vitamin D levels helps you tolerate the drug better. It’s a theory that gained traction after a 2009 study found that 92% of patients with statin-related muscle pain felt better after taking vitamin D supplements. That got a lot of attention. Clinicians started checking vitamin D levels in patients who couldn’t handle statins. Some even began supplementing before trying statins again.
But here’s the problem: the science has split in two directions.
What the Observational Studies Said
Before 2022, most of the evidence came from observational studies-looking back at patient records, not testing in controlled trials. These studies consistently found a pattern: patients with low vitamin D (<20 ng/mL) who had muscle pain from statins often tolerated the drugs again after their levels were corrected.
A 2017 study followed 123 patients who had previously stopped statins due to muscle symptoms. Nearly all of them had vitamin D levels below 20 ng/mL. After giving them 1,000 to 5,000 IU of vitamin D daily for 2 to 8 weeks, 90% were able to restart a statin without muscle pain. That’s a huge number. Even more telling: patients with levels above 20 ng/mL had only a 33% success rate after supplementation. The difference was statistically significant.
Another study from 2015 tracked 34 statin-intolerant patients who got vitamin D to bring their levels above 30 ng/mL. Over 50% of them were able to use a statin again for at least four months. That’s not a small win-especially when you consider most of these patients had tried and failed with two or three different statins before.
Some doctors noticed something else: not all statins behaved the same. Pravastatin and rosuvastatin seemed easier to tolerate after vitamin D correction. One lipid specialist reported that after correcting vitamin D deficiency, he could get 8 out of 10 patients back on statins-something he couldn’t do before.
And then there’s the psychological angle. Patients who know they’re fixing a deficiency feel more in control. One doctor noted that correcting vitamin D made patients more willing to try statins again. It wasn’t just biology-it was trust. If you believe a simple fix is in place, you’re more likely to stick with the treatment.
The Big Study That Changed Everything
In 2022, the JAMA Cardiology study dropped like a bomb. It wasn’t a small observation. It was a randomized, double-blind, placebo-controlled trial with over 2,000 participants. That’s the gold standard. And the results? No difference.
People who took 2,000 IU of vitamin D daily were just as likely to develop muscle pain as those who took a sugar pill. Same rate of muscle symptoms: 31%. Same rate of quitting statins: 13%. No benefit. Not even a hint.
This wasn’t a fluke. The VITAL trial was massive, well-funded by the NIH, and designed specifically to answer this exact question. If vitamin D helped, this study should have found it. It didn’t.
So why did earlier studies show such strong results? The answer might lie in bias. In observational studies, people who get their vitamin D checked and corrected are often more health-conscious. They may eat better, exercise more, or see their doctor more often. These habits alone could improve muscle symptoms-not the vitamin D. Also, muscle pain from statins is subjective. It’s hard to measure. One person’s “ache” is another person’s “cramp.” Without blinding, it’s easy to see improvement where none exists.
Could Statins Be Raising Vitamin D Instead?
Here’s a twist: what if statins are actually increasing vitamin D levels? A 2019 study found that people taking statins had higher vitamin D levels than those who weren’t. That’s the opposite of what you’d expect if statins were causing deficiency.
One theory? Statins might affect how the body processes vitamin D through liver enzymes. Or maybe people who take statins are more likely to get tested and supplemented. The direction of cause isn’t clear. And that’s a problem for the whole hypothesis.
What Should You Do?
So where does this leave you-if you’re on a statin and have muscle pain?
First, don’t panic. Muscle pain from statins is common, but it’s not always the drug’s fault. Other things-like thyroid issues, low potassium, or even overexertion-can cause similar symptoms. Talk to your doctor before making any changes.
Second, testing your vitamin D level is still reasonable. It’s cheap, safe, and worth checking if you’re deficient. If your level is below 20 ng/mL, correcting it is a good idea anyway-for bone health, immune function, and general muscle strength. But don’t assume it will fix your statin pain.
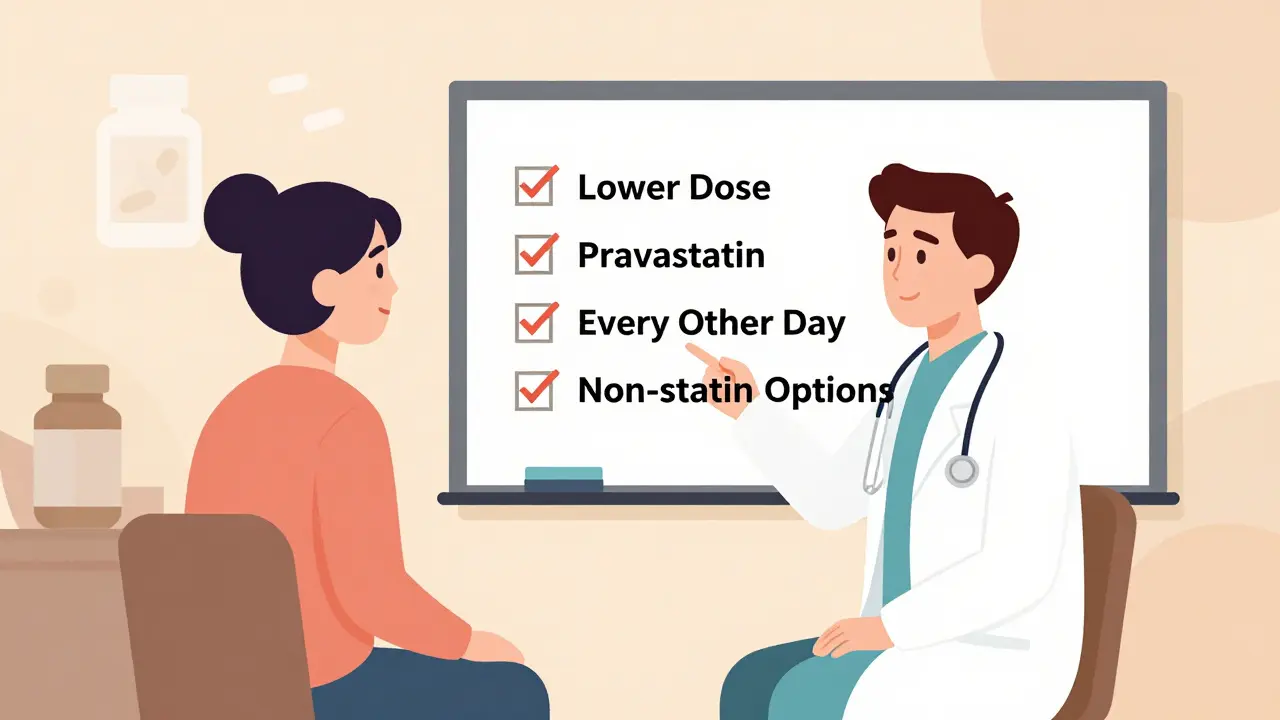
If you’re trying to get back on a statin after stopping due to muscle pain, here’s what actually works:
- Try a lower dose
- Switch to pravastatin or rosuvastatin-they’re less likely to cause muscle issues
- Take statins every other day instead of daily
- Consider non-statin options like ezetimibe or PCSK9 inhibitors if needed
Supplementing vitamin D might help you feel better overall. But don’t count on it to make statins tolerable. The best evidence says it won’t.
Why This Matters Beyond Muscle Pain
Statin intolerance isn’t just about discomfort. It’s about risk. People who stop statins have a 25 to 35% higher chance of having a heart attack or stroke. That’s not a small trade-off.
If we can keep people on statins-even if it’s just by improving their confidence-we save lives. That’s why the vitamin D question mattered so much. It felt like a simple solution to a huge problem.
But science doesn’t care how convenient a theory is. It cares what the data says. And right now, the data says vitamin D doesn’t reliably fix statin intolerance.
That doesn’t mean you shouldn’t care about your vitamin D. You should. But don’t use it as a magic fix for statin side effects. Focus on what does work: the right statin, the right dose, and open communication with your doctor.
What’s Next?
The debate isn’t over. Some researchers still believe there’s a subgroup-maybe people with severe deficiency (below 15 ng/mL)-who might benefit. But no one’s proven it yet. Future studies will need to be even more targeted, with strict definitions of muscle pain and precise vitamin D thresholds.
For now, the message is clear: vitamin D supplementation won’t turn a statin-intolerant patient into a statin-tolerant one. But checking your levels? Still a good idea. Just don’t expect it to solve everything.


Post A Comment