Medication Risk Checker for Kidney Inflammation
Assess Your Risk
This tool estimates your potential risk of developing acute interstitial nephritis based on medications you're taking. AIN is a serious kidney inflammation condition often triggered by common drugs.
Your Risk Assessment
Key Symptoms to Watch For
- Decreased urine output (without dehydration)
- Unexplained fever (37.5-38.5°C)
- Rash (often non-itchy)
- Flank pain (below ribs)
- General malaise (feeling unwell)
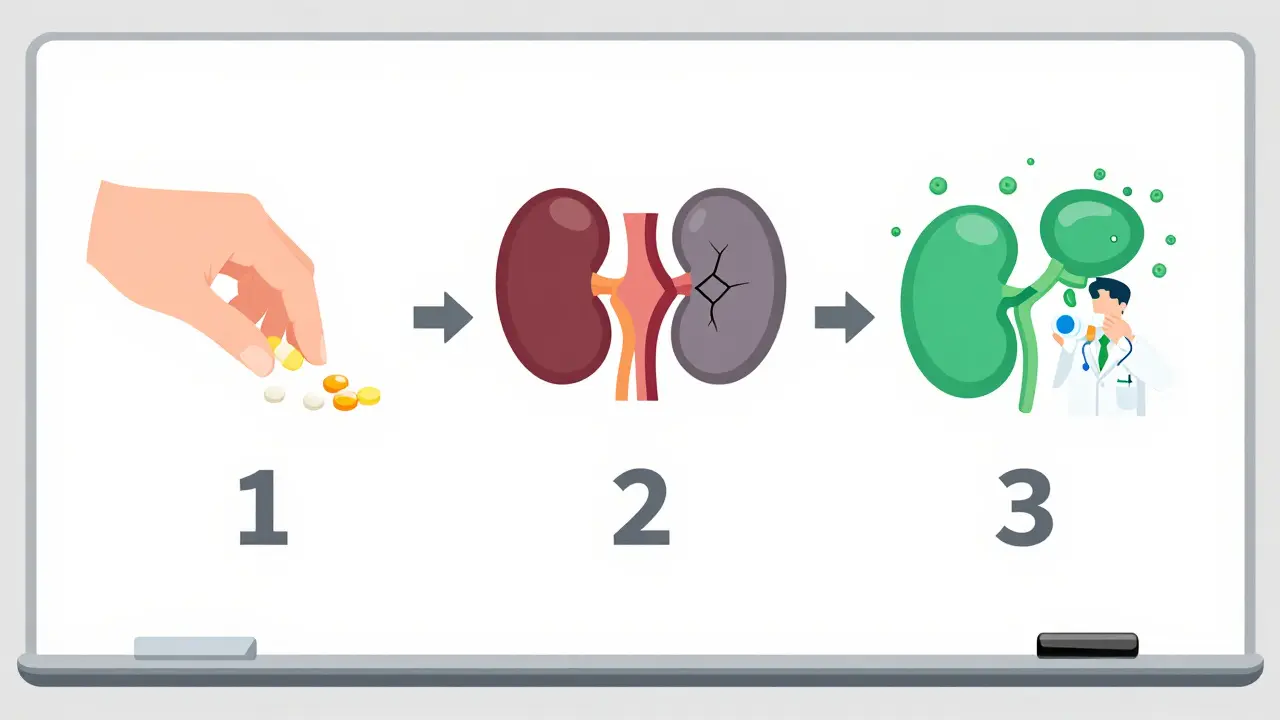
When your kidneys suddenly stop working right, it’s not always a mystery. Sometimes, the cause is something you took for a headache, heartburn, or infection. Acute interstitial nephritis (AIN) is a type of kidney inflammation triggered by medications - and it’s more common than most people realize. Unlike sudden kidney failure from dehydration or severe infection, AIN happens because your immune system reacts to a drug, turning your kidney’s inner tissue into a battleground. The good news? If caught early, it’s often reversible. The bad news? Most people don’t recognize the signs until it’s too late.
What Actually Happens in Your Kidneys?
Your kidneys don’t just filter waste. They also regulate fluids, balance electrolytes, and help control blood pressure. Between the tiny tubes (tubules) that process urine lies the interstitium - a space filled with connective tissue and blood vessels. When a drug like an antibiotic, proton pump inhibitor (PPI), or NSAID triggers an allergic-type reaction, immune cells flood this area. It’s like your body mistakes part of your kidney for a virus. The swelling blocks urine flow, and your kidney function drops fast.This isn’t just theoretical. In Australia, as in the U.S. and Europe, drug-induced AIN now accounts for nearly 1 in 5 cases of unexplained acute kidney injury in hospitals. The most common culprits? Antibiotics (especially penicillin and ciprofloxacin), PPIs like omeprazole and pantoprazole, and over-the-counter painkillers like ibuprofen and naproxen. Even a single dose can set it off - though most cases appear after weeks or months of use.
The Hidden Symptoms - Not Just Swelling or Fatigue
Most people think kidney problems mean swollen legs, dark urine, or extreme tiredness. But AIN often hides behind subtler signs:- Decreased urine output - You’re not peeing as much, even if you’re drinking normally.
- Fever - Unexplained low-grade fever (37.5-38.5°C) that lasts days.
- Rash - Not always itchy or red. Sometimes just a faint, flat patch on your chest or arms.
- Flank pain - Dull ache just below your ribs on one or both sides.
- General malaise - Feeling "off" without a clear reason, like the flu but no cough or sore throat.
Here’s the catch: the classic triad of rash, fever, and eosinophilia (high white blood cells) only shows up in fewer than 10% of cases. That means if you don’t have all three, it doesn’t rule out AIN. In fact, many patients are misdiagnosed with urinary tract infections because they have sterile pyuria - white blood cells in the urine without bacteria. That’s a red flag.
Which Medications Are Most Likely to Cause It?
Not all drugs carry the same risk. Some are far more dangerous than others:| Drug Class | Examples | Typical Onset | Recovery Rate |
|---|---|---|---|
| Antibiotics | Penicillin, ampicillin, ciprofloxacin | 1-3 weeks | 80-90% |
| Proton Pump Inhibitors (PPIs) | Omeprazole, pantoprazole, esomeprazole | 10-24 weeks | 60-70% |
| NSAIDs | Ibuprofen, naproxen, diclofenac | 3-6 months | 70-80% |
| Immune Checkpoint Inhibitors | Pembrolizumab, nivolumab | 2-12 weeks | 50-60% |
PPIs are especially sneaky. People take them for months for heartburn, assuming they’re harmless. But studies show PPI-induced AIN now causes over 12 cases per 100,000 people each year - and the number is rising. In fact, from 2005 to 2020, hospitalizations for drug-induced AIN jumped by over 200%. Older adults on multiple medications are at highest risk. If you’re over 65 and on three or more drugs daily, your risk is nearly five times higher.

How Doctors Diagnose It - And Why It’s Often Missed
There’s no single blood test for AIN. Diagnosis relies on a chain of clues:- Urinalysis - Look for sterile pyuria (white blood cells without infection) and eosinophils in the urine (present in 30-70% of cases).
- Blood tests - Rising creatinine (≥0.3 mg/dL in 48 hours) confirms acute kidney injury.
- Kidney biopsy - The only way to confirm AIN. It shows immune cells swelling the tissue between tubules. This is done when suspicion is high, usually within 3-7 days of symptom onset.
- Timeline review - Did you start a new drug within the last 3 months? That’s the golden window.
Here’s where things go wrong: many doctors don’t think of AIN unless the patient has a rash or fever. But in over half of cases, those signs are absent. A 2023 study found that 65% of patients were initially told they had a UTI or dehydration. One man in Sydney was treated for "gout" for weeks before his kidney biopsy revealed AIN from long-term ibuprofen use.
Treatment - Stop the Drug, Then What?
The most important step? Stop the drug immediately. Waiting even a few extra days increases the chance of permanent damage. In fact, studies show that if you stop the medication within 72 hours of suspicion, recovery chances jump from 60% to over 85%.But stopping the drug isn’t always enough. About 30-70% of patients need corticosteroids - usually prednisone - to calm the inflammation. The debate is ongoing. Some nephrologists give steroids right away. Others wait to see if kidney function improves on its own. The European guidelines recommend steroids if creatinine hasn’t improved after 7 days. The American guidelines are stricter - only if creatinine is above 3.0 mg/dL.
Recovery time varies. Younger people often bounce back in 6-8 weeks. Older adults may take 3-4 months. Some never fully recover. About 15-25% of untreated cases develop permanent kidney damage. A few end up on dialysis.
Who’s Most at Risk?
It’s not random. Certain patterns show up again and again:- Age over 65 - 65% of cases occur in this group.
- On five or more medications - Polypharmacy increases risk 4.7-fold.
- Women - 1.8 times more likely than men to develop AIN.
- Chronic NSAID or PPI users - Especially those with arthritis, GERD, or heart disease.
And here’s something few know: genetic factors play a role. A specific gene variant - HLA-DRB1*03:01 - makes people 4.2 times more likely to develop AIN from PPIs. Testing for this isn’t routine yet, but research is moving fast.
What You Can Do Right Now
You don’t need to be a doctor to protect your kidneys. Here’s what works:- Keep a full medication list - Include OTC drugs, supplements, and herbal remedies. Show it to every new doctor.
- Ask: "Could this hurt my kidneys?" Especially if you’re over 50 or on multiple drugs.
- Don’t ignore unexplained fatigue or reduced urination - Especially if you’ve started a new drug.
- Get a basic kidney test - A simple blood test for creatinine and eGFR can catch early problems.
- Review PPI use - If you’ve been on omeprazole for over 3 months, ask if you still need it.
There’s no magic pill. But awareness saves kidneys. The rise in AIN isn’t random - it’s tied to how often we take drugs without thinking about long-term effects. Your kidneys don’t scream until they’re almost broken. Pay attention to the whispers.
Can you get acute interstitial nephritis from over-the-counter painkillers?
Yes. NSAIDs like ibuprofen, naproxen, and diclofenac are responsible for 15-20% of all medication-induced AIN cases. The risk increases with long-term use - especially if taken daily for 3-6 months. People over 50 with arthritis or back pain are most vulnerable. Stopping the drug early usually leads to recovery, but some develop lasting kidney damage.
Is acute interstitial nephritis permanent?
Not always. If caught early and the triggering drug is stopped within 72 hours, most people recover kidney function fully. But if diagnosis is delayed beyond 2-3 weeks, up to 25% develop permanent kidney damage. Older adults and those with other health conditions (like diabetes or heart disease) are more likely to have lasting effects. Regular kidney function checks after recovery are essential.
Do all cases of AIN require a kidney biopsy?
No, but it’s the only way to confirm the diagnosis. Biopsy is recommended when AIN is strongly suspected - especially if urine tests show sterile pyuria or eosinophils, creatinine is rising, and a new drug was started within the last 3 months. In some cases, doctors may try stopping the drug first and monitor recovery. If kidney function doesn’t improve in 5-7 days, biopsy becomes necessary to rule out other causes.
Can proton pump inhibitors (PPIs) really cause kidney damage?
Yes. PPIs like omeprazole are now the second-leading cause of AIN, after antibiotics. Studies show they can trigger kidney inflammation after just 10-12 weeks of use. The FDA added a warning label in 2021. Many patients take PPIs for years for mild heartburn - but the risk doesn’t disappear over time. If you’re over 65 or on multiple medications, ask your doctor if you still need it.
How long does it take to recover from AIN?
Recovery time depends on age, how quickly the drug was stopped, and how much damage was done. Younger patients (under 50) often recover in 6-8 weeks. Older adults (over 65) may take 12-16 weeks. If steroids are needed, recovery can take 3-4 months. Some people never return to 100% kidney function. Regular follow-up blood tests are crucial to track progress and prevent long-term decline.

