When you vomit something that looks like coffee grounds, or pass black, tarry stools, it’s not just a bad stomach bug. It’s a medical emergency called upper GI bleeding. This isn’t rare-it happens to about 100 out of every 100,000 adults each year in the U.S. And if you’re over 80, your risk jumps to 300 per 100,000. The truth? Many people ignore the signs until they collapse. But knowing what’s happening and acting fast can save your life.
What Exactly Is Upper GI Bleeding?
Upper GI bleeding means blood is coming from somewhere in your upper digestive tract: your esophagus, stomach, or the first part of your small intestine (duodenum). It’s not a disease itself-it’s a symptom of something serious underneath. The most common causes? Peptic ulcers, swollen veins in the esophagus (varices), and irritation from medications like NSAIDs or blood thinners.Peptic ulcers alone cause 40-50% of cases. These are open sores in the lining of your stomach or duodenum, often from H. pylori bacteria or long-term use of ibuprofen or aspirin. Esophageal varices, which happen in people with advanced liver disease, account for 10-20% of cases. These veins swell under pressure from liver scarring and can rupture without warning. And then there are the less common but still dangerous causes: tears in the esophagus (Mallory-Weiss), severe gastritis, and even stomach cancer.
How Do You Know You’re Bleeding?
The symptoms are hard to miss-if you know what to look for.- Hematemesis: Vomiting bright red blood or material that looks like dark coffee grounds. That dark color means the blood has been sitting in your stomach and started to break down.
- Melena: Black, sticky, foul-smelling stools. This isn’t from eating beets or iron pills. It’s digested blood. If you notice this, don’t wait.
- Hematochezia: Bright red or maroon stools. This usually means a massive bleed-blood is moving too fast to get digested.
- Physical signs: Dizziness, fainting, rapid heartbeat (over 100 bpm), low blood pressure (below 90 systolic), pale skin, and extreme fatigue. These mean your body is losing blood faster than it can compensate.
A 2023 study from the Praram 9 Heart and Vascular Institute showed that patients who waited more than 12 hours after symptoms started to seek help had nearly double the risk of dying. That’s why recognizing these signs early is critical.
The Glasgow-Blatchford Score: Your First Triage Tool
Not every case needs an ambulance. But how do you tell who’s in real danger? Doctors use the Glasgow-Blatchford score-a simple checklist based on six objective numbers:- Hemoglobin level (below 12.9 g/dL for men, below 11.9 g/dL for women)
- Systolic blood pressure (below 100 mmHg)
- Pulse rate (above 100 bpm)
- Presence of melena
- History of syncope (fainting)
- History of liver or heart disease
If your score is 2 or higher, you need hospital care. A score of 0 or 1? You might be safe to go home after evaluation. A 2019 study of over 3,000 patients confirmed this system correctly identified 85% of people who needed urgent treatment-and spared 15% from unnecessary hospital stays.
Dr. Robert Logan from Harvard says this tool has changed the game. Before it, everyone with bleeding went to the ER. Now, doctors can focus resources on those who truly need them.
What Happens in the ER?
When you arrive, the first priority isn’t finding the source-it’s keeping you alive. This is called stabilization.Step one: Check your vital signs. Are you dizzy? Is your heart racing? Is your blood pressure dropping? If yes, you get oxygen and IV fluids immediately.
Step two: Blood tests. A complete blood count (CBC) tells you how low your hemoglobin is. A BUN-to-creatinine ratio above 30:1 is a strong indicator of upper GI bleeding-68.8% accurate, according to a 2021 study in the Annals of Internal Medicine.
Step three: Blood transfusion. If your hemoglobin is below 7 g/dL, or you’re showing signs of shock (cold skin, confusion, low urine output), you’ll get packed red blood cells. Each unit raises your hemoglobin by about 1 g/dL. But don’t overdo it-target 7-9 g/dL. Going higher doesn’t help and might even hurt.
Step four: Start PPIs. Even before endoscopy, you’ll get an 80mg IV bolus of a proton pump inhibitor (like pantoprazole), followed by a continuous 8mg/hour drip. This isn’t just to reduce stomach acid-it actually helps stop bleeding by improving clot stability. The 2022 COBALT trial showed this cuts rebleeding rates in half-from 22.6% down to 11.6%.
Endoscopy: The Critical Diagnostic and Treatment Step
The only way to know exactly where the bleeding is coming from is through an esophagogastroduodenoscopy (EGD). And timing matters. The American College of Gastroenterology recommends it within 24 hours. But if you’re high-risk, aim for 12 hours-or sooner.A 2022 study showed that getting endoscopy within 12 hours reduces death rates by 25% compared to waiting longer. That’s the difference between walking out of the hospital and not making it.
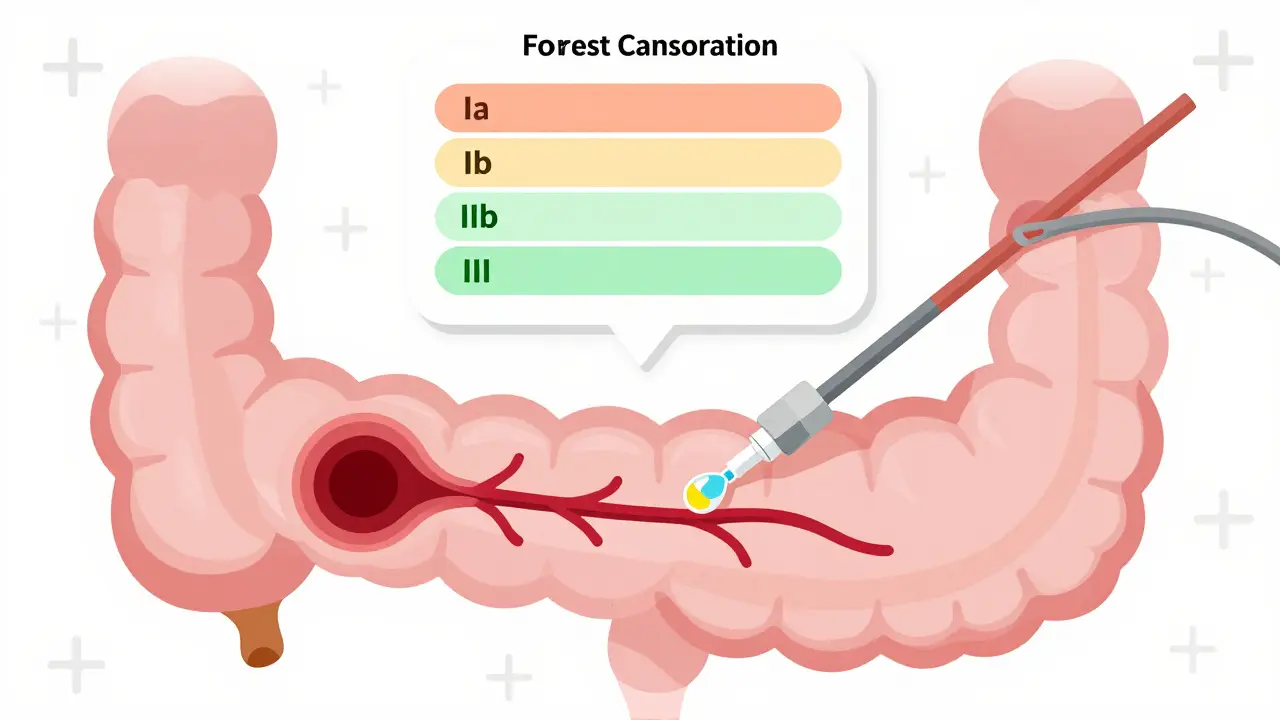
During the procedure, doctors use the Forrest classification to judge how dangerous the bleeding is:
- Class Ia: Blood spurting out. 90% chance of rebleeding without treatment.
- Class Ib: Blood oozing. 50% rebleeding risk.
- Class IIa: A visible blood vessel. Also 50% risk.
- Class IIb: A clot on top. Lower risk, but still needs monitoring.
- Class III: No active bleeding. Low risk.
For non-variceal bleeding (like ulcers), doctors use a combination of epinephrine injections and either heat probes or hemoclips. This stops bleeding in 90-95% of cases. For varices, they use band ligation-tiny rubber bands slipped around the swollen veins. It’s far better than older methods like injecting chemicals (sclerotherapy), which had higher complication rates.
Variceal Bleeding: A Different Beast
If your bleeding comes from esophageal varices, the approach changes. You’re not just bleeding-you’re bleeding because your liver is failing. This is life-threatening.First, give vasoactive drugs. Either terlipressin (2mg IV, then every 4-6 hours) or octreotide (50mcg IV bolus, then 50mcg/hour). These drugs shrink the swollen veins and reduce pressure.
Second, give antibiotics. Ceftriaxone 1g IV daily. Why? Because patients with liver disease are extremely vulnerable to infections when they bleed. Antibiotics cut mortality by 25%.
Third, band ligation within 24 hours. Studies show it reduces rebleeding from 60% to just 25% in the first few weeks.
And here’s the kicker: Even after the bleeding stops, you’re not out of the woods. Up to 20% of people with variceal bleeding die within six weeks. That’s why long-term care-beta-blockers, regular endoscopies, and liver evaluation-is non-negotiable.
What You Shouldn’t Do
There are dangerous myths out there.- Don’t wait to see if it “goes away.” One Reddit user, u/StomachSOS, had black stools dismissed as “iron supplements” for two weeks-until he collapsed. His hemoglobin was 5.8. He needed a transfusion. He almost died.
- Don’t assume PPIs fix everything. Dr. Elena Rodriguez from Johns Hopkins warns that 30% of low-risk patients get unnecessary PPIs because doctors skip endoscopy. You can’t treat what you haven’t diagnosed.
- Don’t restart NSAIDs. A 2022 JAMA study found that people on SSRIs (like antidepressants) have double the risk of GI bleeding. NSAIDs? Same story. If you’ve had a bleed, talk to your doctor before taking ibuprofen, naproxen, or even low-dose aspirin again.
Recovery and Prevention
After you’re stable, recovery is about more than just healing the bleed. It’s about preventing the next one.A 2022 University of Michigan study tracked 1,200 patients after discharge. Two-thirds felt anxious about it happening again. Over 40% changed their diet-cutting out coffee, alcohol, spicy food. Over 30% stopped NSAIDs on their own, without medical advice. That’s risky. You need a plan.
For ulcers: Test for H. pylori. If positive, take antibiotics and a PPI for 14 days. Avoid NSAIDs. If you need pain relief, use acetaminophen instead.
For varices: Take beta-blockers like propranolol to lower pressure in the veins. Get endoscopic surveillance every 1-2 years. If your liver is failing, consider a transplant evaluation.
For everyone: Quit smoking. Limit alcohol. Don’t ignore new abdominal pain or fatigue. These aren’t just “aging” symptoms-they could be warning signs.
The Future Is Here
New tools are making diagnosis faster and more accurate.In 2023, the FDA approved Hemospray, a powder that’s sprayed directly onto bleeding sites during endoscopy. It forms a physical barrier and works even when the area is hard to reach. In trials, it stopped bleeding in 92% of tough cases.
Even more exciting? AI-assisted endoscopy. A 2023 trial called ENDOSCAPE showed AI systems spotted subtle bleeding signs with 94.7% accuracy-compared to 78.3% for human doctors. That’s huge. But there’s a catch: These AI tools were trained mostly on data from white patients. They’re 15% less accurate in Black and Hispanic populations, according to Dr. Susan Chang at Stanford. This isn’t science fiction-it’s happening now. And it’s not fair.
Meanwhile, the NIH’s UGIB-360 study, launched in January 2024, is tracking 10,000 people to build personalized risk models using genetics, gut bacteria, and lifestyle. Results are expected by late 2025. The goal? Predict who’s most likely to bleed before it happens.
What You Can Do Today
If you’ve had a GI bleed, or know someone who has:- Know the signs: coffee-ground vomit, black stools, dizziness.
- Don’t delay. Go to the ER if you suspect bleeding.
- Ask for the Glasgow-Blatchford score. It’s standard now.
- Insist on endoscopy within 12 hours if you’re high-risk.
- Follow up. This isn’t a one-time fix. It’s a chronic condition that needs ongoing care.
Upper GI bleeding doesn’t care if you’re busy, scared, or think it’s “just heartburn.” It’s silent until it’s not. But with the right knowledge and quick action, you can beat it.
What does coffee-ground vomit mean?
Coffee-ground vomit means blood has been in your stomach long enough to be partially digested by stomach acid. It’s a classic sign of upper GI bleeding, often from a peptic ulcer or gastritis. It’s not normal and requires immediate medical attention.
Can you have an upper GI bleed without vomiting blood?
Yes. Many people only notice black, tarry stools (melena) or feel dizzy and weak without vomiting. This is especially common in older adults or those on blood thinners. The absence of vomiting doesn’t mean the bleeding isn’t serious.
Is upper GI bleeding fatal?
It can be. The mortality rate is around 8-10% overall, but jumps to 20% for variceal bleeding and over 30% in patients over 80. Early treatment reduces death risk significantly. Delaying care is the biggest risk factor.
Do I need to stop my blood thinners if I have a GI bleed?
Never stop them on your own. Your doctor will weigh the risk of rebleeding against the risk of a clot (like a stroke or heart attack). In many cases, they’ll restart anticoagulants within days-once the bleeding is controlled. This decision is individualized and requires expert guidance.
How long does it take to recover from an upper GI bleed?
Most people are stable within 2-5 days, but full recovery takes weeks. Your hemoglobin will rebound slowly-about 1 g/dL per week. You’ll need follow-up endoscopy to confirm healing. Avoid alcohol, NSAIDs, and smoking for at least 4-6 weeks. Long-term management depends on the cause-ulcers may need ongoing PPIs; varices require lifelong monitoring.
Can stress cause an upper GI bleed?
Stress doesn’t directly cause ulcers, but it can worsen them. Severe physical stress-like from major surgery, burns, or critical illness-can lead to stress-related mucosal damage and bleeding. Emotional stress alone isn’t a direct cause, but it can lead to behaviors (like drinking, skipping meals, or using NSAIDs) that increase risk.


Post A Comment