Vitamin D Therapy: Basics, Benefits, and How to Get It Right
When working with Vitamin D Therapy, the use of vitamin D supplements or prescribed forms to correct deficiency, support bone health, and manage related conditions. Also known as vitamin D supplementation, it plays a crucial role in many body systems. Vitamin D therapy isn’t just a pill; it’s a strategy that ties together nutrition, labs, and lifestyle.
Most people start because their blood test shows low 25‑hydroxyvitamin D. Low levels can cause fatigue, muscle aches, and bone thinning. To fix that, you need enough Calcium, the mineral that works hand‑in‑hand with vitamin D to build and maintain strong bones. Without calcium, even the best vitamin D dose won’t improve bone density. This makes the link between the two nutrients a core part of any therapy plan.
When calcium and vitamin D are in balance, the parathyroid glands stay calm. In chronic kidney disease or other conditions, patients often develop Secondary Hyperparathyroidism, a state where the glands overproduce parathyroid hormone due to low calcium or vitamin D. Targeted vitamin D therapy can lower that hormone level, easing bone loss and calcification risks. So, managing secondary hyperparathyroidism is a major reason doctors prescribe active forms of vitamin D.
Kidney function matters a lot. The kidneys activate vitamin D, converting it to the form the body can use. If kidney disease is present, doses may need to be higher or use of calcitriol (the active form) is preferred. Regular lab checks, especially serum calcium and phosphate, guide safe dosing and prevent complications like vascular calcification.
Beyond labs, the ultimate goal is better Bone Health, the strength and structure of the skeleton, which depends on the vitamin D‑calcium partnership. Adequate therapy reduces fracture risk, supports healing after injury, and helps older adults maintain mobility. Think of bone health as the visible outcome of the biochemical dance between vitamin D, calcium, and the parathyroid system.
Choosing the right dose starts with the form of vitamin D. Vitamin D3 (cholecalciferol) is most effective for most adults, while D2 (ergocalciferol) is used in some prescriptions. Weekly or monthly high‑dose regimens work for people who struggle with daily pills. The key is to aim for a serum level of 30–50 ng/mL, which many guidelines flag as optimal. Testing before and after a few months of therapy tells you if you’ve hit the target.
Watch out for drug interactions. Steroids, anticonvulsants, and some weight‑loss meds can speed up vitamin D breakdown, making you need higher doses. Conversely, excess calcium supplements can push calcium too high when combined with aggressive vitamin D therapy. Always tell your doctor about every prescription and over‑the‑counter product you use.
Practical tips: get safe sun exposure (10‑15 minutes on arms and face a few times a week), choose a supplement that lists the IU amount clearly, and take it with a fatty meal for better absorption. Set a reminder in your phone, and keep a log of your lab results so you can see progress over time.
What You’ll Find Below
Below is a curated list of articles that dive deeper into each of these topics. You’ll see guides on how to time your doses, how calcium and vitamin D work together, ways to manage secondary hyperparathyroidism, and specific advice for patients with kidney disease. Whether you’re just starting therapy or looking to fine‑tune an existing plan, the posts ahead give actionable insights you can apply right away.
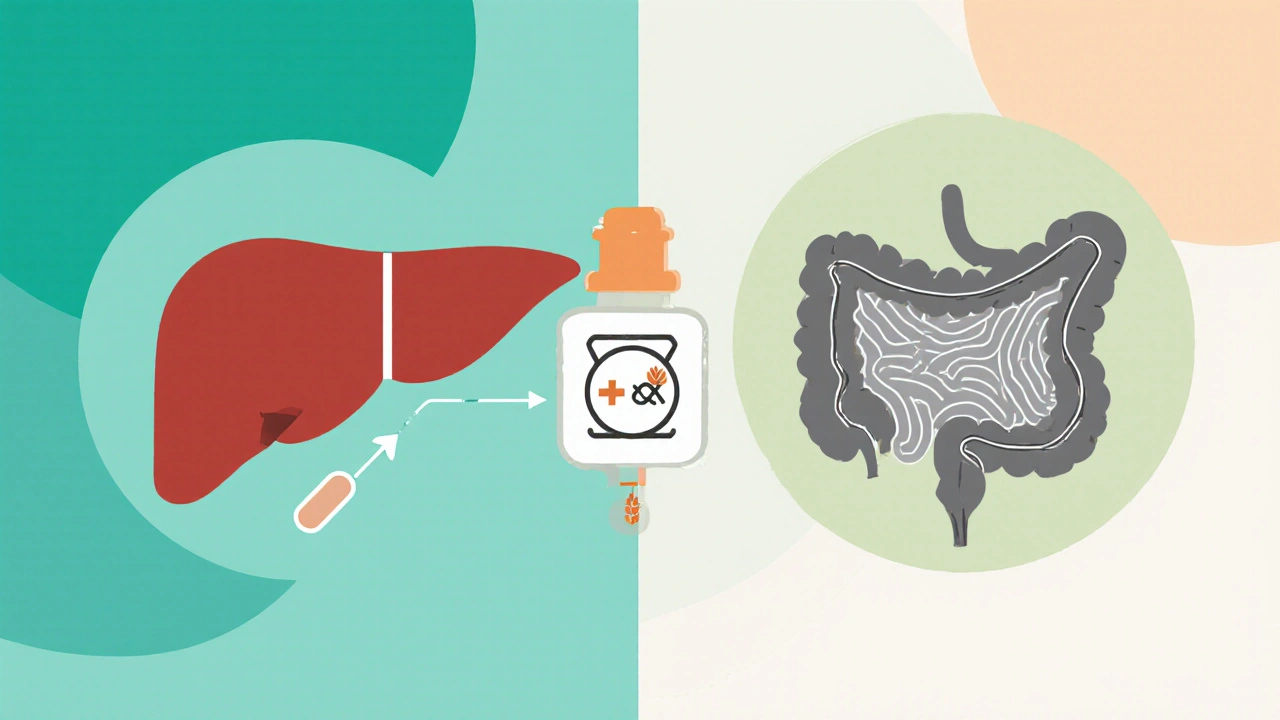
How Alfacalcidol Helps Patients with Celiac Disease - Benefits and Practical Guide
Discover how alfacalcidol improves calcium absorption, bone health, and overall wellbeing for celiac patients, with dosing tips, safety advice, and a handy comparison table.
Read More