Shellfish allergy isn’t just about avoiding shrimp or crab. For millions of people, it’s a daily balancing act between enjoying meals and avoiding life-threatening reactions. The real danger isn’t always what’s on the plate-it’s what’s hidden in the sauce, the oil, or even the air. And here’s the twist: you might test positive for shellfish allergy without ever having a reaction. That’s because of cross-reactivity-a confusing, often misunderstood phenomenon that trips up patients and doctors alike.
What Makes Shellfish So Dangerous?
Shellfish allergy is triggered by proteins in marine invertebrates, not by toxins or contaminants. The main culprit is tropomyosin, a protein found in muscle tissue. It’s heat-stable, meaning frying, boiling, or grilling won’t destroy it. That’s why even cooked shellfish can cause reactions. Tropomyosin is also found in dust mites and cockroaches, which is why people allergic to these common household pests often test positive for shellfish-even if they’ve never eaten it.Studies show that 68% of people with dust mite allergies have IgE antibodies to shellfish, but only about 20% of them actually react when they eat it. This is called sensitization without clinical allergy. It’s why blood tests alone can’t be trusted. A positive test doesn’t always mean you’re allergic. It just means your immune system recognizes the protein. The real test? What happens when you eat it.
Which Shellfish Are Cross-Reactive?
Not all shellfish are created equal. There are two main groups: crustaceans (shrimp, crab, lobster, crawfish) and mollusks (clams, oysters, scallops, mussels). Cross-reactivity is high within crustaceans. If you’re allergic to shrimp, you have a 75-92% chance of reacting to crab or lobster. That’s because their tropomyosin proteins are nearly identical-95%+ match in amino acid sequence.But mollusks? Different story. Only 15-20% of people allergic to crustaceans react to clams or mussels. The proteins are different enough that many can eat them safely. A 2019 study in the Journal of Allergy and Clinical Immunology found that people with shrimp allergy who avoided mollusks unnecessarily could safely add them back into their diet after proper testing.
This is where component-resolved diagnostics come in. Instead of testing for whole shellfish extract, doctors now test for specific proteins like tropomyosin, sarcoplasmic calcium-binding protein (SCBP), and arginine kinase. If your IgE is only reacting to tropomyosin and you have dust mite allergy, you might be fine with mollusks. If your IgE is reacting to SCBP, you’re at higher risk for severe reactions-even with small amounts.

Why Restaurants Are the Biggest Risk
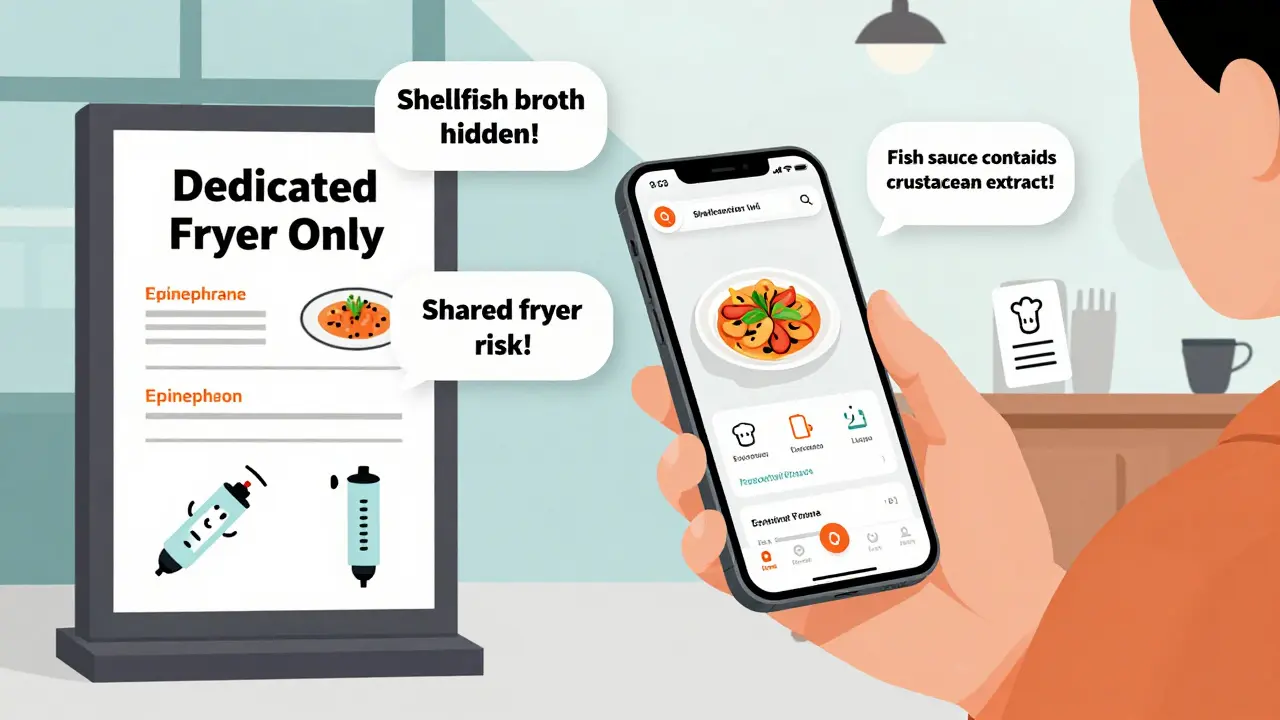
A 2022 survey by the Asthma and Allergy Foundation of America found that 68% of people with shellfish allergy had an accidental exposure while eating out. Of those, 22% needed epinephrine. The most dangerous places? Seafood restaurants, where 87% of reactions happen. But surprisingly, Asian restaurants account for 41% of reactions-not because they serve more shellfish, but because shellfish is hidden in sauces, broths, and seasonings.Crab or shrimp paste is often used in Thai, Chinese, and Vietnamese dishes to add umami. You won’t find it listed as “shellfish” on the menu. It’s labeled as “fish sauce,” “oyster sauce,” or “seafood extract.” Even if you avoid shrimp, you might still be eating it. And then there’s the oil. A 2019 study showed that 63% of crustacean reactions happen because of shared fryers. Fries cooked in the same oil as shrimp? That’s enough to trigger a reaction.
Server knowledge is shockingly low. A 2023 National Restaurant Association study found only 37% of servers could correctly identify shellfish ingredients on a menu. Many confuse “gluten-free” with “allergy-safe.” They assume if something doesn’t have wheat, it’s safe. It’s not. And language barriers make it worse. In 32% of reactions at ethnic restaurants, communication failed because staff didn’t understand the severity.
How to Eat Out Safely
You don’t have to give up dining out. You just need a strategy.- Call ahead. Don’t wait until you arrive. Call 24 hours in advance and ask to speak with the chef. Ask: “Do you use shellfish in any sauces, broths, or oils?” Many restaurants will make accommodations if they know you’re coming.
- Use a chef card. These are printed cards that list your allergies in clear, simple language. The Food Allergy Research & Education (FARE) card is available in 15 languages. Hand it to the chef, not the server. Studies show 92% of allergists recommend this method.
- Avoid shared fryers. Ask: “Is there a dedicated fryer for gluten-free or allergen-free items?” If they say no, walk away. Cross-contact in oil is one of the most common causes of reactions.
- Use apps like AllergyEats or Nosh List. These apps let users report which restaurants are safe. Nosh List has over 120,000 user reviews and flags dishes with hidden shellfish.
- Don’t rely on “no shellfish” on the menu. That doesn’t mean no shellfish in the kitchen. Ask what’s in the seasoning, broth, and garnishes.
One Reddit user, u/AllergyWarrior42, shared: “I only eat at places with dedicated fryers. That one change cut my reactions by 80%.” Another, u/NutFreeChef, said: “I ask to speak with the chef. If they get annoyed, I go somewhere else. My life is worth it.”
Testing and Diagnosis: Don’t Trust the Blood Test Alone
Many people are told they’re allergic to shellfish because of a blood test. But here’s the truth: false positives are common. A 2025 study in Frontiers in Allergy found that 60% of positive shellfish IgE tests in dust mite-allergic patients were false. That means they were sensitized, not allergic.The gold standard is still the oral food challenge-eating a small amount of shellfish under medical supervision. But that’s risky and expensive. That’s why component-resolved diagnostics are changing the game. Tests like ImmunoCAP ISAC 112, approved by the FDA in 2024, can tell you exactly which proteins you’re reacting to. If your IgE is only to tropomyosin and you have dust mite allergy, you might not need to avoid all shellfish. If you’re reacting to SCBP or arginine kinase, you need to be much more careful.
Dr. Scott Sicherer from Mount Sinai says: “Tropomyosin-specific testing reduces false positives by 35-40%. That means fewer people are unnecessarily avoiding food they can safely eat.”
What’s Next? The Future of Shellfish Allergy Management
The field is moving fast. In January 2024, a Phase 2 clinical trial at Mount Sinai showed that peptide immunotherapy could desensitize 70% of shrimp-allergic patients. That’s not a cure, but it could mean fewer reactions and less fear.AI is also stepping in. AllergyMapper, a beta app launched in March 2024, scans restaurant menus and flags hidden shellfish ingredients. It’s 85% accurate so far. As global shellfish production grows-up 53% since 2010-so does the risk. Climate change is even altering the protein profiles in shellfish, which could make allergies worse in the future.
For now, the best tools are knowledge, communication, and preparation. Carry your epinephrine. Know your triggers. Ask the hard questions. And remember: you’re not being difficult-you’re being smart.
Can you outgrow a shellfish allergy?
Unlike milk or egg allergies, shellfish allergy is usually lifelong. Only about 5-10% of people outgrow it, and it’s rare in adults. Most people who develop shellfish allergy in their 30s or 40s keep it for life. Regular testing and food challenges under medical supervision are the only way to know if tolerance has changed.
Is it safe to eat imitation crab if I’m allergic to shellfish?
No. Imitation crab is made from surimi, which is processed white fish, but it often contains shellfish extracts or is made on shared equipment. Many brands use crab flavoring derived from real shellfish. Even if the label says “no shellfish,” cross-contact is likely. Unless the product is certified allergen-free and made in a dedicated facility, avoid it.
Can I eat seaweed or sushi if I have a shellfish allergy?
Seaweed itself is safe-it’s a plant, not an animal. But sushi is risky. Many rolls contain crab, shrimp, or fish sauce. Even plain sushi rice can be cooked with dashi, a broth made from dried fish or shellfish. Always ask how the rice is prepared. Opt for simple options like plain tuna or avocado rolls, and tell the chef you have a shellfish allergy.
Do I need to avoid iodine if I have a shellfish allergy?
No. This is a myth. Shellfish allergy is not related to iodine. Iodine is an element found in many foods, including dairy, eggs, and table salt. People with shellfish allergy can safely receive iodine-based contrast dye for CT scans or X-rays. Studies have shown no increased risk of reaction in these patients.
What should I do if I accidentally eat shellfish?
If you have epinephrine, use it immediately. Don’t wait for symptoms to get worse. Call 911 even if you feel better after the shot-symptoms can return. Antihistamines like Benadryl help with mild symptoms like hives, but they won’t stop anaphylaxis. Always carry two epinephrine auto-injectors. One might not be enough.
Are there any new treatments on the horizon?
Yes. Peptide immunotherapy for shrimp allergy showed 70% success in reducing sensitivity in a 2024 clinical trial. It’s not available yet, but Phase 3 trials are planned. Oral immunotherapy (OIT) for shellfish is also being tested, though results are mixed. For now, avoidance and emergency preparedness remain the standard of care.


Post A Comment