High blood pressure in people over 65 isn’t just a number on a chart-it’s a daily risk that can lead to strokes, heart attacks, and kidney damage. When doctors prescribe a combo pill that mixes olmesartan amlodipine, they’re trying to hit two targets at once: blocking the hormone that narrows vessels and relaxing the smooth muscle in the arterial wall. But seniors aren’t the same as younger adults; they process drugs differently, they take more meds, and they’re more vulnerable to drops in blood pressure. This guide walks you through everything you need to know about using this powerful duo safely in the older population.
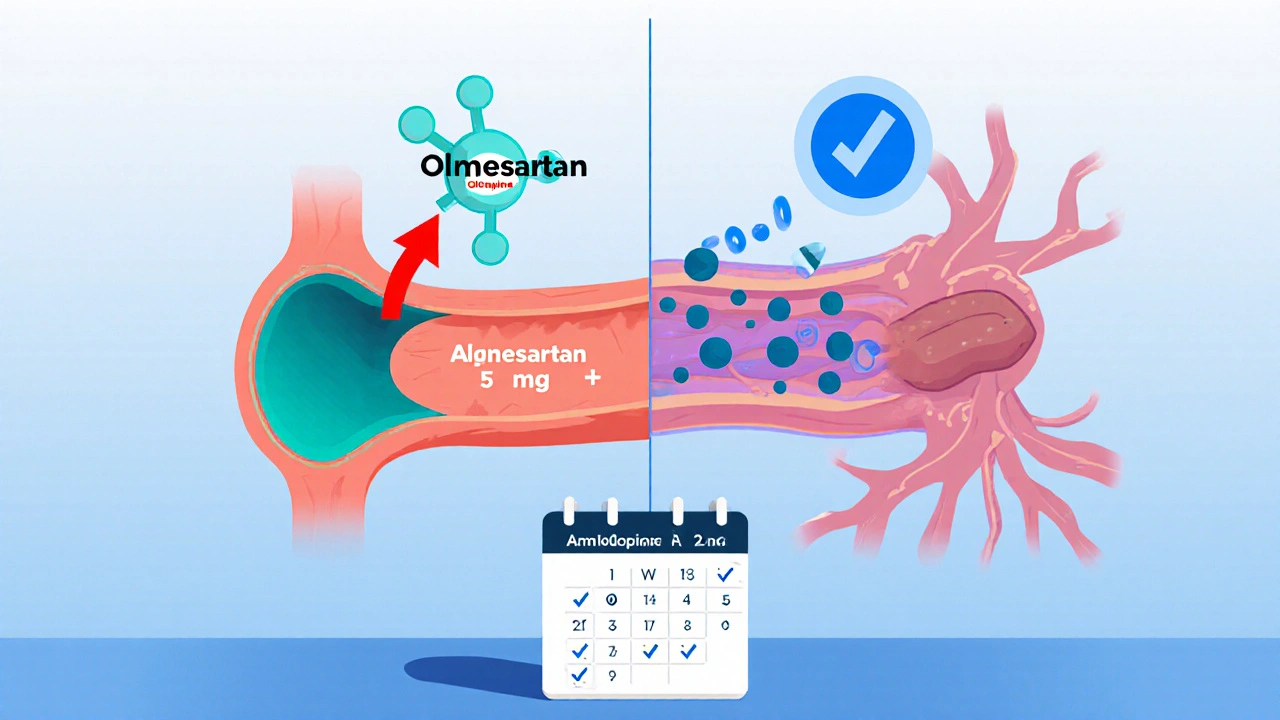
What the Two Drugs Do - Mechanism in Plain Language
Olmesartan is an angiotensin II receptor blocker (ARB) that stops a hormone called angiotensin II from tightening blood vessels. By keeping the vessels relaxed, the heart doesn’t have to work as hard, and blood pressure drops.
Amlodipine is a calcium‑channel blocker (CCB). It prevents calcium from entering the smooth muscle cells of arteries, which also keeps them wide and flexible. When you pair an ARB with a CCB, you get a double‑hit that tackles high blood pressure from two angles, often allowing a lower dose of each and reducing side‑effects.
Why Seniors Need a Different Approach
The body changes after 65. Liver metabolism slows, kidney filtration drops, and the baroreflex that keeps blood pressure steady becomes less responsive. These shifts mean that a dose that works fine for a 45‑year‑old could cause dizziness, fainting, or a dangerous fall in an 80‑year‑old.
Key factors to consider:
- Reduced renal clearance: Both drugs are eliminated partially by the kidneys. A lower glomerular filtration rate (GFR) can let the medication build up.
- Altered plasma protein binding: Older adults often have less albumin, which can increase the free (active) fraction of the drug.
- Polypharmacy: The average senior takes 8‑12 prescription meds, raising the chance of drug‑drug interactions.
Starting Dose and Titration for the Elderly
Guidelines suggest beginning at the lowest possible dose and titrating up only if blood pressure stays above target (usually < 130/80 mmHg for most seniors). A typical starting regimen looks like:
- Olmesartan 5 mg + Amlodipine 2.5 mg once daily.
- Monitor blood pressure and symptoms for 2‑4 weeks.
- If systolic pressure remains >140 mmHg, increase to Olmesartan 10 mg + Amlodipine 5 mg.
Never jump more than one dose step; gradual increases let the body adapt and give clinicians a chance to catch side‑effects early.
Common Side‑Effects in Older Adults and How to Manage Them
Both drugs are generally well‑tolerated, but seniors report a few patterns more often.
- Orthostatic hypotension: A sudden drop in blood pressure upon standing. Teach patients to rise slowly, check standing BP, and consider a bedtime dose if dizziness occurs at night.
- Peripheral edema: Amlodipine can cause fluid buildup in the ankles. Reduce sodium intake, elevate legs, or add a low‑dose thiazide diuretic if needed.
- Hyperkalemia: ARBs can raise potassium, especially when kidney function is impaired. Routine labs every 3‑4 weeks during dose changes are essential.
- Renal function decline: Slight rises in serum creatinine are expected, but an increase >30 % warrants dose reduction or discontinuation.
Lab Monitoring Checklist
| Test | Frequency | Target Range |
|---|---|---|
| Serum Creatinine & eGFR | Baseline, then every 3 months | eGFR ≥60 mL/min/1.73 m² (ideal) |
| Serum Potassium | Baseline, 2 weeks after dose change, then quarterly | 3.5‑5.0 mmol/L |
| Blood Pressure (sitting & standing) | Weekly for first month, then monthly | Sitting <130/80 mmHg; standing drop ≤20 mmHg |
| Liver enzymes (ALT/AST) | Baseline, then annually | Within normal limits |
Drug Interactions to Watch Out For
Because seniors often juggle many prescriptions, a few interactions stand out:
- NSAIDs (e.g., ibuprofen, naproxen): Can blunt the antihypertensive effect and worsen kidney function.
- Potassium‑sparing diuretics (e.g., spironolactone): Heighten risk of hyperkalemia when combined with an ARB.
- Other antihypertensives: Adding a beta‑blocker or ACE inhibitor may cause excess blood pressure drop; adjust doses.
- Grapefruit juice: Inhibits CYP3A4 metabolism of amlodipine, raising its plasma level.
When possible, aim for the simplest regimen: a single‑pill combination plus one or two other agents at the lowest effective doses.
Practical Tips for Clinicians and Caregivers
- Assess frailty: Use tools like the Clinical Frailty Scale before starting therapy. Very frail patients may need even lower initial doses.
- Educate on self‑monitoring: Provide a home blood pressure cuff and a log sheet. Encourage recording lying, sitting, and standing readings.
- Address adherence: The combo pill reduces pill burden, but confusion can arise from similar‑looking tablets. Use clear labeling and color‑coded blister packs.
- Review medication list every 6 months: Look for over‑the‑counter drugs, supplements, or recent prescriptions that could interact.
- Plan for falls: If a patient reports dizziness, consider lowering the dose or switching the amlodipine component to a shorter‑acting CCB.
Comparison: Olmesartan vs. Other ARBs for the Elderly
| ARB | Half‑life (hours) | Typical Dose for Seniors | Renal Clearance % | Notable Side‑effects |
|---|---|---|---|---|
| Olmesartan | 13‑15 | 5‑20 mg daily | 30‑35 | Rare cough, hyperkalemia |
| Losartan | 6‑9 | 25‑50 mg daily | 30‑35 | Higher incidence of dizziness |
| Valsartan | 6‑9 | 80‑160 mg daily | 30‑40 | Edema, mild renal impact |
| Telmisartan | 24 | 20‑80 mg daily | 60‑70 | Potential for higher potassium |
Frequently Asked Questions
Can a senior take the combo pill with a diuretic?
Yes, many clinicians pair the combo with a low‑dose thiazide diuretic to improve blood pressure control. Start the diuretic at 2.5 mg hydrochlorothiazide and watch for increased urination or electrolyte shifts.
What should I do if I feel faint after the first week?
Sit or lie down immediately, elevate the legs, and check your blood pressure standing up. Contact your doctor; you may need the dose lowered or the timing shifted to bedtime.
Is it safe to drink grapefruit juice while on amlodipine?
Avoid grapefruit juice. It can raise amlodipine levels and increase the risk of low blood pressure and swelling.
How often should kidney function be checked?
At baseline, then every 3 months after any dose change, and at least twice a year if renal function is stable.
Can I stop the medication if my blood pressure improves?
Never stop abruptly. Speak with your physician; they may taper the dose slowly and monitor for rebound hypertension.
Bottom Line for Seniors and Caregivers
The olmesartan/amlodipine combo offers a powerful, once‑daily solution that fits nicely into a busy senior’s routine. Success hinges on starting low, watching labs, and staying alert to dizziness or swelling. With careful monitoring and clear communication, most older adults can achieve target blood pressure without compromising safety.

Post A Comment