When you’re diagnosed with sleep apnea, your doctor might recommend a breathing device. Two names come up most often: CPAP and BiPAP. They both help you breathe better at night, but they’re not the same. Choosing the wrong one can mean discomfort, poor sleep, or even wasted money. So what’s the real difference? And more importantly-which one is actually right for you?
How CPAP Works and Who It’s For
CPAP stands for Continuous Positive Airway Pressure. It’s been the gold standard for treating obstructive sleep apnea since the early 1980s. The machine delivers a single, steady stream of air pressure through a mask while you sleep. That pressure keeps your airway open so you don’t stop breathing.
Most people with obstructive sleep apnea (OSA) start with CPAP. In fact, about 85-90% of OSA patients are treated with it. It’s simple, effective, and widely covered by insurance. Typical pressure settings range from 4 to 20 cm H₂O, adjusted based on your sleep study results.
CPAP machines like the ResMed AirSense 11 or Philips DreamStation 2 are designed for ease of use. They have ramp features that slowly increase pressure as you fall asleep, built-in humidifiers to prevent dryness, and automatic leak detection. Many users report noticeable improvements in sleep quality within days.
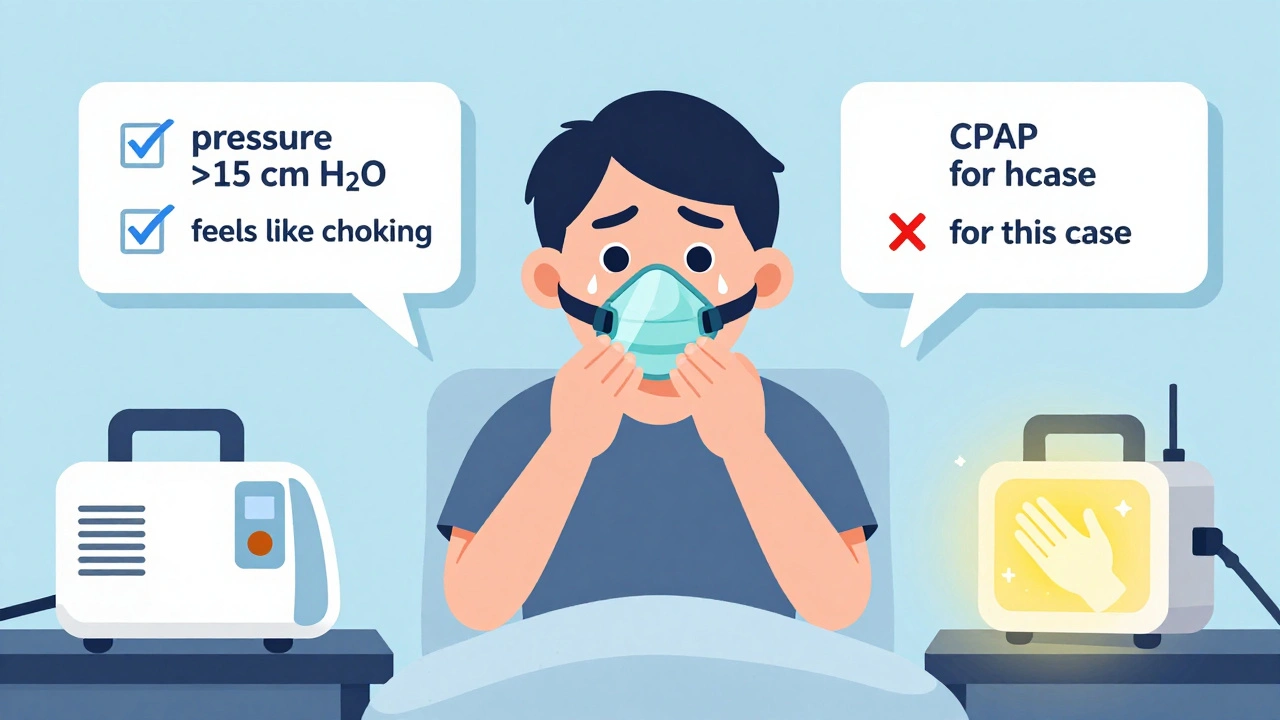
But CPAP isn’t perfect. If you need high pressure-say, 15 cm H₂O or more-exhaling against that constant force can feel like breathing through a straw. That’s where some people struggle. It’s not the machine’s fault. It’s just that the design doesn’t adapt to your natural breathing rhythm.
How BiPAP Works and Why It’s Different
BiPAP, or Bilevel Positive Airway Pressure, gives you two different pressure levels: one for inhaling (IPAP) and a lower one for exhaling (EPAP). Think of it like a breathing partner who pushes air in when you need it and eases up when you breathe out.
This difference matters. For someone struggling with high CPAP pressure, switching to BiPAP can cut the effort of exhaling by 30-40%. That’s not a small comfort-it’s the difference between tolerating therapy and actually sticking with it.
BiPAP machines also have advanced features CPAP doesn’t. Many include a backup rate: if you stop breathing for a few seconds, the machine will deliver a breath automatically. This is critical for people with central sleep apnea or neuromuscular diseases like ALS or Parkinson’s, where the brain doesn’t always signal the lungs to breathe.
BiPAP settings are more complex. IPAP usually ranges from 8 to 30 cm H₂O, and EPAP from 4 to 25 cm H₂O. There needs to be at least a 3 cm H₂O difference between them for the machine to work properly. These settings aren’t guessed at-they’re fine-tuned during a sleep study that often takes longer than a standard CPAP titration.
When BiPAP Is the Better Choice
BiPAP isn’t better for everyone. In fact, for most people with simple obstructive sleep apnea, it offers no real advantage over CPAP. A 2021 Cochrane review of over 1,800 patients found no significant difference in sleep quality, adherence, or daytime alertness between CPAP and BiPAP for standard OSA.
But BiPAP shines in specific situations:
- High-pressure needs: If your CPAP pressure is 15 cm H₂O or higher, BiPAP can make breathing feel natural again.
- COPD with hypercapnia: If you have chronic lung disease and high carbon dioxide levels in your blood, BiPAP helps your lungs clear CO₂ more effectively.
- Obesity hypoventilation syndrome: People with a BMI over 30 who also have daytime drowsiness and high CO₂ levels benefit from BiPAP’s support.
- Central sleep apnea: This isn’t caused by a blocked airway-it’s when your brain forgets to tell your lungs to breathe. BiPAP’s backup breath feature saves lives here.
- Neuromuscular disorders: Conditions like muscular dystrophy or spinal cord injuries weaken breathing muscles. BiPAP can take over some of that work.
According to the American Thoracic Society, BiPAP is the recommended first-line treatment for all of these conditions-not because it’s stronger, but because it’s smarter for those specific problems.
Cost, Insurance, and Real-World Barriers
CPAP machines cost between $500 and $1,200. BiPAP devices? They’re $800 to $1,800. That’s not just a price difference-it’s a barrier.
Insurance doesn’t treat them equally. Medicare, for example, will cover 80% of CPAP costs right away. But for BiPAP? You have to prove CPAP didn’t work. That means you need to show you used CPAP for 30 days, at least 4 hours a night, and still couldn’t tolerate the pressure-usually because it was over 15 cm H₂O.
That’s a tough hurdle. Many patients give up on CPAP before they even get to that point. But if you’re one of the 10-15% who truly need BiPAP, the extra cost and paperwork are worth it.
Even then, there’s a catch. BiPAP machines are more complex. About 34% of BiPAP users report trouble with settings or mode confusion, compared to just 18% of CPAP users. A 2022 survey found 27% of BiPAP users experienced “machine cycling issues”-where the device doesn’t sync with their breathing, causing jerky or forced breaths.
That’s why professional setup matters. While many CPAP users learn to manage everything themselves, BiPAP often requires help from a respiratory therapist, especially when using S/T (spontaneous/timed) mode.
User Experiences: What People Really Say
On forums like Reddit’s r/CPAP, stories are split. One user, u/SleepWarrior2022, wrote: “BiPAP at 14/8 felt like breathing normally. CPAP at 14 felt like choking.” That’s a common theme among those who needed high pressure.
But others say the opposite. A 2023 survey of over 12,000 users found CPAP users reported higher satisfaction (78% vs. 72%) and easier use (71% rated ease of use as excellent, compared to 58% for BiPAP). Why? Simplicity. If you don’t need the extra features, BiPAP just feels like overkill.
There’s also a psychological factor. People who switch from CPAP to BiPAP often feel like they’ve been “upgraded.” But if they didn’t need it, the machine’s complexity can make them anxious. One user on Sleep Review Magazine’s forum said: “I spent two weeks trying to understand the modes. I just wanted to sleep.”
What Happens After You Start?
Both devices require adjustment. Most people need 2-4 weeks to get used to CPAP. BiPAP? That can stretch to 3-6 weeks. Why? More settings, more variables, more things that can go wrong.
Insurance companies require you to use your device at least 4 hours a night for 70% of nights in the first 3 months to keep coverage. About 65% of CPAP users hit that mark. BiPAP users? Only 60%. That’s not because BiPAP doesn’t work-it’s because it’s harder to use correctly.
Mask fit is the #1 reason people quit both devices. A 2023 study found 70% of initial discomfort comes from poor mask sealing-not the machine itself. So whether you choose CPAP or BiPAP, investing in a good mask fitting session is non-negotiable.
What’s New in 2025?
Technology hasn’t stood still. ResMed’s AirCurve 10 VAuto (2023) uses AI to adjust pressure in real time based on your breathing patterns. Philips’ DreamStation 3 now includes built-in oxygen monitoring. These aren’t just gimmicks-they’re tools that help personalize therapy.
But here’s the catch: insurance doesn’t always cover these upgrades. And many of these “smart” features are only available on BiPAP models. That’s driving adoption in complex cases, but it’s also creating confusion. Are you getting advanced tech because you need it-or because it’s being sold to you?
Experts agree: BiPAP adoption will grow by 15-20% annually through 2027, mainly because of aging populations and rising obesity rates. But a 2023 Health Affairs study warned that $420 million is wasted every year in the U.S. because BiPAP is prescribed for simple OSA cases that don’t need it.
How to Decide: A Simple Checklist
Still unsure? Ask yourself these questions:
- Was your sleep study diagnosis simple obstructive sleep apnea (no central apnea, no COPD, no neuromuscular disease)? → Go with CPAP.
- Did your doctor recommend CPAP pressure above 15 cm H₂O? → Consider BiPAP.
- Do you feel like you’re fighting the machine when you exhale? → BiPAP may help.
- Do you have other health conditions like COPD, heart failure, or ALS? → BiPAP is likely needed.
- Are you overwhelmed by settings and modes? → CPAP is simpler and just as effective for most.
If you’re still stuck, ask for a trial. Some providers offer short-term rentals of both devices. Try each for a week. Sleep with them. See which one feels like breathing-instead of fighting it.
Final Thought: It’s Not About the Machine-It’s About the Fit
There’s no “best” device. There’s only the right one for you. CPAP is the workhorse. BiPAP is the specialist. One isn’t superior-it’s just different.
For 9 out of 10 people with sleep apnea, CPAP is enough. It’s proven, affordable, and effective. For the other 1 in 10-those with complex breathing issues, high pressure needs, or neurological conditions-BiPAP isn’t just helpful. It’s essential.
Don’t let marketing or peer pressure push you into a device you don’t need. And don’t give up on CPAP too soon. Many people who say they “can’t tolerate” it just need better mask fit, humidity control, or a few weeks to adjust.
Your sleep matters. Choose wisely-not because it’s the most advanced, but because it’s the one that lets you breathe easily, every night.
Is BiPAP better than CPAP for sleep apnea?
Not for most people. CPAP is the first-line treatment for obstructive sleep apnea and works just as well as BiPAP for simple cases. BiPAP is only better if you need higher pressure, have central sleep apnea, COPD, obesity hypoventilation, or a neuromuscular disorder. For standard OSA, BiPAP adds cost and complexity without improving outcomes.
Can I switch from CPAP to BiPAP if I’m not comfortable?
Yes-but only after trying to fix the issue first. Most discomfort comes from mask fit, humidity settings, or not giving yourself time to adjust. If you’ve used CPAP for at least 30 days, at 4+ hours per night, and still can’t tolerate the pressure (especially above 15 cm H₂O), talk to your sleep doctor about switching to BiPAP. Insurance often requires this documentation before approving the change.
Does BiPAP cure sleep apnea?
No device cures sleep apnea. Both CPAP and BiPAP treat it by keeping your airway open during sleep. They don’t fix the root cause-like excess weight, jaw structure, or neurological signals. But they do prevent dangerous breathing pauses, reduce daytime fatigue, and lower your risk of heart disease and stroke. Consistent use is what matters.
How long does it take to get used to BiPAP?
Most people need 3 to 6 weeks to adjust to BiPAP, compared to 2 to 4 weeks for CPAP. The extra settings, dual pressure levels, and backup breath features can feel strange at first. Work with your respiratory therapist to fine-tune the pressure difference and ramp settings. Don’t give up before the 3-week mark-your body needs time to adapt.
Will insurance cover BiPAP if I just want it?
No. Medicare and most private insurers require proof that CPAP didn’t work before approving BiPAP. That means documented use of CPAP for at least 30 days, at least 4 hours per night, and a pressure setting of 15 cm H₂O or higher that you couldn’t tolerate. BiPAP isn’t a luxury upgrade-it’s a medical necessity for specific conditions.
Can I use BiPAP for snoring without sleep apnea?
No. BiPAP is a medical device approved only for diagnosed sleep-disordered breathing conditions like obstructive or central sleep apnea, COPD with hypercapnia, or obesity hypoventilation. Snoring alone doesn’t qualify. Using a BiPAP machine without a prescription is unsafe and illegal. If you snore but don’t have apnea, talk to your doctor about other options like oral appliances or lifestyle changes.
Are there side effects to using BiPAP?
Side effects are similar to CPAP: dry mouth, nasal congestion, mask leaks, and skin irritation. But because BiPAP has more complex settings, users may also experience discomfort from mismatched pressure levels, machine cycling issues, or feeling like the device is breathing for them. These problems usually fix themselves with proper setup and adjustment by a trained therapist.
How often do I need to replace my BiPAP machine?
Most insurance plans cover a new machine every 5 years, assuming it’s still working properly. Manufacturers typically design these devices to last 5-7 years with regular maintenance. Replace masks, tubing, and filters every 3-6 months. If your machine is over 5 years old and you’re having frequent errors, poor sleep, or inconsistent pressure delivery, it’s time for a replacement.


Post A Comment