If your medicine shows up on a recall list, don’t panic - but don’t ignore it either. Every year, thousands of medications are pulled from shelves because of contamination, labeling errors, or manufacturing flaws. In 2022 alone, the FDA issued over 4,800 recalls. Most aren’t life-threatening, but some are. The difference between staying safe and risking harm comes down to what you do in the next 24 hours.
Don’t Stop Taking Your Medicine Right Away
This is the biggest mistake people make. If you find out your blood pressure pill, diabetes medication, or antidepressant is being recalled, your first instinct might be to toss it and go without. That’s dangerous. Abruptly stopping certain drugs can cause seizures, spikes in blood pressure, or even heart attacks. The FDA’s 2021 valsartan recall specifically warned patients: "Continue taking your medicine until you talk to your doctor or pharmacist." The recall isn’t about the drug being ineffective - it’s about a possible contaminant or mislabeling. Your condition still needs treatment. Stopping suddenly creates a new, avoidable risk.Check Your Lot Number and Expiration Date
Not every bottle of a recalled drug is affected. Only specific batches are. That’s why you need to look at the lot number printed on the box or bottle. It usually looks like a mix of letters and numbers - for example, AB123C45 or L789-22. Compare it to the list on the FDA’s website. If your lot number matches, your medicine is in the recall. If it doesn’t, you’re safe to keep using it. About 45% of patients assume the whole brand is recalled, but that’s rarely true. The FDA requires manufacturers to list exact lot numbers, NDC codes, and expiration dates in every recall notice. Don’t guess - check.Contact Your Pharmacy Immediately
Your pharmacist is your best ally during a recall. Most pharmacies have automated systems that flag recalled medications when a prescription is filled. But if you’re unsure, call them. Ask: "Is my medication on a recall list? Is my lot number affected?" Pharmacists can confirm within minutes and often have replacement bottles ready from unaffected batches. According to the American Pharmacists Association, 92% of pharmacies can provide a new supply within 24 to 48 hours. They can also help you switch to an alternative brand if needed. Don’t wait for your doctor’s office to call - pharmacies are on the front lines of this process.Know the Recall Class - But Don’t Wait to Act
The FDA classifies recalls into three levels:- Class I: Highest risk. Could cause serious injury or death. About 15% of recalls fall here. Common examples: contaminated antibiotics or mislabeled insulin.
- Class II: Moderate risk. Might cause temporary health issues or reversible side effects. Most recalls are here - about 70%.
- Class III: Lowest risk. Unlikely to cause harm. Often just labeling errors, like wrong dosage printed.
Even if your recall is Class II or III, you still need to act. Class I recalls demand immediate replacement. But Class II recalls are often the most dangerous because people think they’re "not serious" and delay. In 2022, 8% of all reported adverse events tied to recalls came from Class II drugs that patients kept using too long.
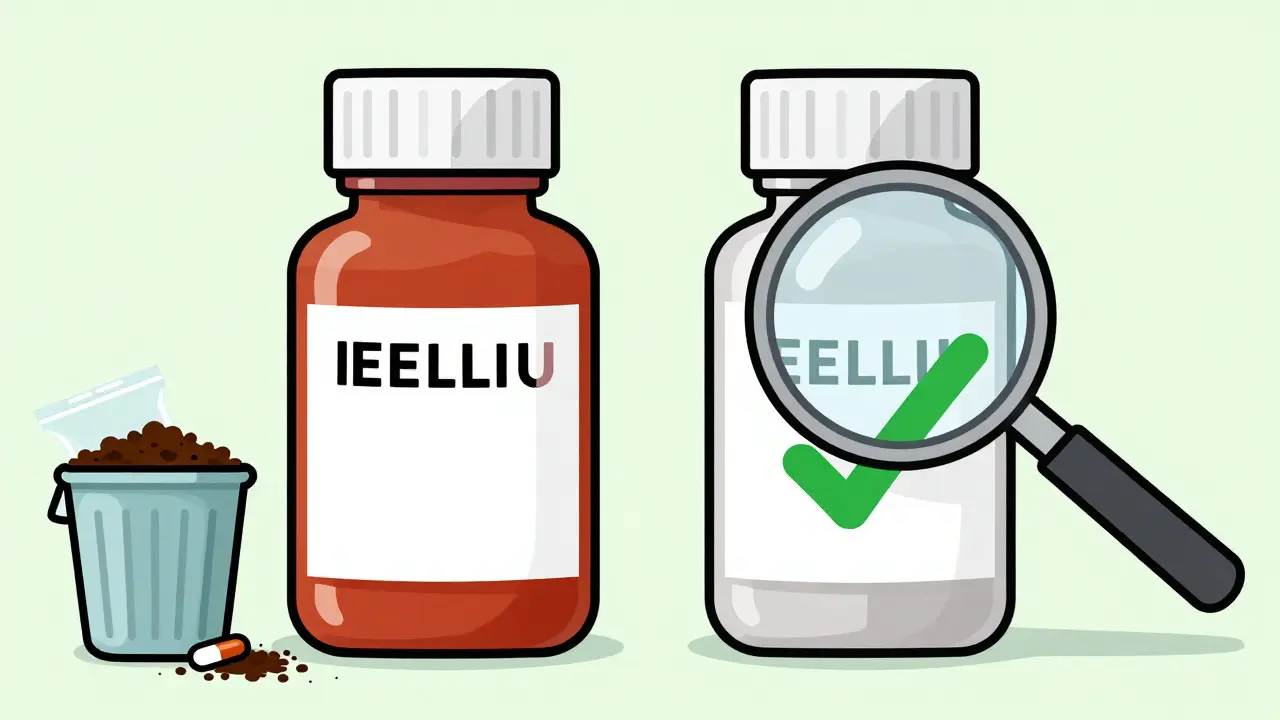
Dispose of Recalled Medication Properly
If you’re told to throw out your medicine, don’t flush it or toss it in the regular trash. That’s unsafe for the environment and risky for kids or pets. The FDA recommends mixing pills with something unappetizing - like used coffee grounds, cat litter, or dirt - then sealing them in a plastic bag. Put that bag in your regular trash. Some pharmacies offer take-back bins. Call ahead to ask. If the recall notice doesn’t say how to dispose of it, ask your pharmacist. Improper disposal is one of the top three mistakes patients make during recalls.Watch for Side Effects and Report Them
If you’ve taken a recalled drug, pay attention to your body. Did you get dizzy? Nauseous? Have unusual bruising? Trouble breathing? These could be signs the medication caused harm. Keep a simple log: date, time, dose, and any symptom. If something feels off, call your doctor. Even if you’re not sure it’s related, report it. The FDA’s MedWatch program received 142,000 patient reports in 2022 - and 27% of those led to new recalls. Your report could help prevent someone else from being hurt.Keep a Medication Log
This is a simple habit that saves time and stress. Write down the name of each prescription, the dose, when you refill it, and the lot number. Keep it in your phone notes or a small notebook. When a recall happens, you can check your list in seconds instead of rummaging through pill bottles. Only 18% of patients do this - but those who do resolve recall issues 60% faster. It’s not just for recalls. It helps during doctor visits, pharmacy questions, and emergency situations.
How to Check for Recalls Yourself
You don’t have to wait for a letter or a call. Go to the FDA’s website and search for recalls. Here’s how:- Visit www.fda.gov/safety/recalls
- Use the search bar to type your drug’s brand name (e.g., "Valsartan")
- Use the "Product Type" filter to select "Human Drugs"
- Click on any matching result to see the full recall notice, including affected lot numbers
You can also sign up for the FDA’s free RSS feed or email alerts. About 45% of healthcare workers use these alerts - you should too. No need to download an app. Just subscribe once, and you’ll get updates directly.
Common Mistakes to Avoid
- Stopping your meds without talking to a professional. This causes more harm than the recall itself.
- Assuming all bottles of the same drug are recalled. Only specific lots are affected.
- Flushing pills or throwing them in the trash without mixing them. Harmful to water supplies and wildlife.
- Waiting for a phone call or letter. Recalls move fast. Check the FDA site yourself.
What’s Being Done to Improve This?
The FDA is working to make recalls faster and more visible. In 2024, they started pilot programs to send recall alerts directly to patients through pharmacy benefit managers and mobile apps. Early results show a 35% improvement in how quickly people respond. They’re also pushing manufacturers to include clearer lot numbers and QR codes on packaging. But until those changes are nationwide, you’re your own best defense.Bottom Line
A medication recall isn’t a crisis - but it’s a prompt. You don’t need to be an expert. You just need to act smart: check your lot number, call your pharmacy, don’t stop your medicine, dispose of it safely, and report anything unusual. Most recalls are resolved in under 10 business days when patients respond quickly. Your next step? Open your medicine cabinet right now. Find your last prescription. Look at the lot number. Write it down. That’s how you protect yourself - one bottle at a time.What should I do if I find out my medicine is recalled?
Don’t stop taking it immediately. Check the lot number against the FDA recall notice. Call your pharmacy to confirm if your specific bottle is affected. They can usually replace it within 24-48 hours. Only stop the medication if your doctor or pharmacist tells you to.
Are all bottles of a recalled drug dangerous?
No. Only specific batches - identified by lot numbers - are affected. Most recalls involve a small percentage of production. Don’t assume your bottle is unsafe just because the drug name is on the list. Always check the lot number.
Can I just throw away recalled medicine in the trash?
No. Flushing or tossing pills directly into the trash can harm the environment and endanger children or pets. Mix them with something unappealing like coffee grounds or cat litter, seal them in a plastic bag, then put them in the regular trash. Ask your pharmacist if they have a take-back program.
Why does the FDA say not to stop taking recalled medication?
For many drugs - especially those for high blood pressure, diabetes, or mental health - stopping suddenly can cause serious health problems like stroke, seizures, or rebound symptoms. The recall is usually about contamination or labeling, not the drug’s effectiveness. Your doctor or pharmacist will help you switch safely.
How do I know if a recall is serious?
The FDA labels recalls as Class I (highest risk), Class II (moderate), or Class III (lowest). Class I recalls could cause serious injury or death and require immediate action. But even Class II and III recalls need attention. Don’t wait to act based on the class - verify your lot number and contact your pharmacy right away.
Can I get a refund or replacement for recalled medicine?
Yes. Most pharmacies will replace recalled medication at no cost. If you paid out-of-pocket, ask your pharmacy about reimbursement. Insurance typically covers replacements. Keep your receipt and the recall notice - you may need them for documentation.
What if I already took a recalled drug and feel fine?
Even if you feel fine, stop using the recalled product and get a replacement. Some side effects may appear later. Keep track of any symptoms - even minor ones - and report them to your doctor. If you’re unsure whether you took a bad batch, call your pharmacy with your lot number.
How often do medication recalls happen?
Over 4,800 drug recalls were issued in 2022 by the FDA. Most are Class II or III - minor issues like mislabeled packaging or incorrect expiration dates. Only about 15% are Class I, which involve serious health risks. Recalls are increasing slightly each year, but the system is designed to catch problems before they cause widespread harm.


Post A Comment