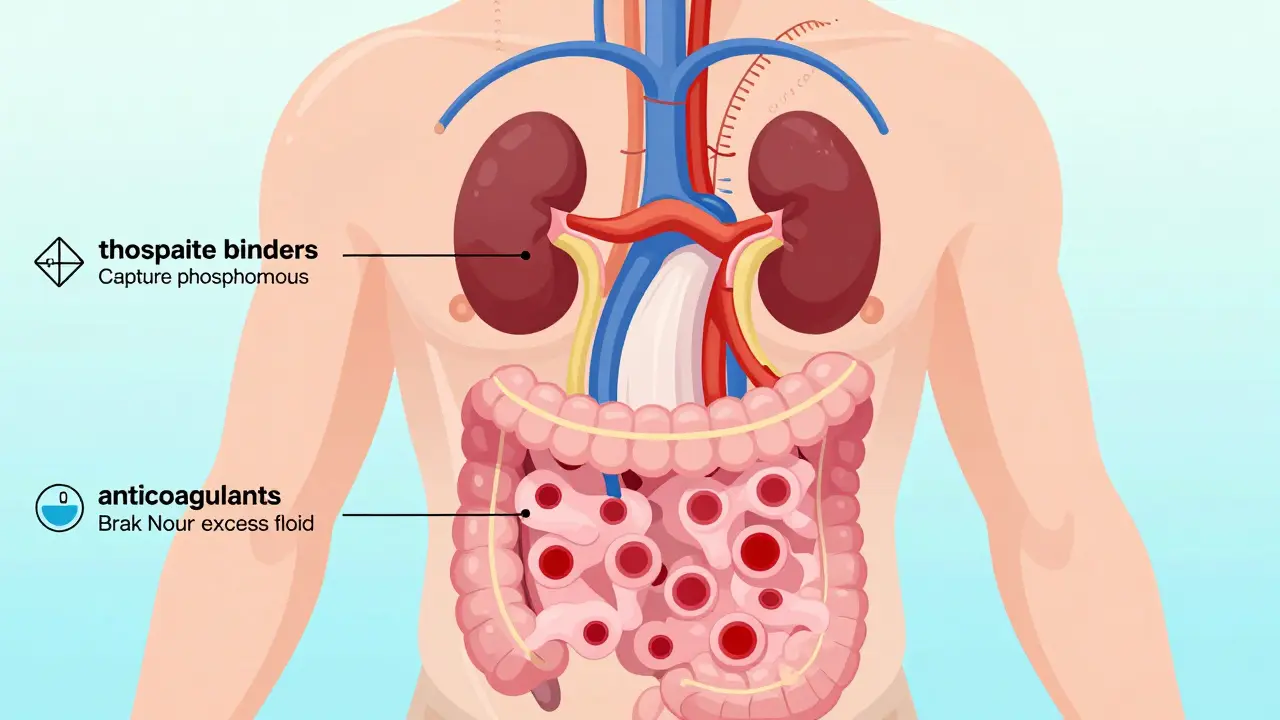
When your kidneys aren’t working right, it’s not just about peeing less or feeling tired. Your whole body gets out of balance. Too much phosphorus builds up. Fluid pools in your legs and lungs. Blood clots become a real danger. That’s where three key types of medications come in: phosphate binders, diuretics, and anticoagulants. These aren’t optional extras. They’re essential tools to keep you alive and out of the hospital.
Phosphate Binders: Stopping Harmful Minerals Before They Absorb
Your kidneys normally flush out excess phosphorus. When they fail, phosphorus piles up in your blood. High levels don’t just hurt your bones-they calcify your arteries, heart valves, and blood vessels. That’s why 60% of people with stage 4 or 5 kidney disease have dangerously high phosphorus, according to the National Kidney Foundation.
Phosphate binders don’t fix your kidneys. They work in your gut. They grab onto the phosphorus from your food and carry it out in your poop instead of letting it enter your bloodstream. You take them with every meal and snack. Miss a dose, and phosphorus slips through.
There are four main types:
- Calcium-based (calcium acetate, calcium carbonate): Cheap, around $50-$80 a month. But they can raise your calcium levels too high, leading to more calcification. Not the first choice anymore.
- Sevelamer (Renagel, Renvela): Doesn’t affect calcium. Reduces mortality by 18% in dialysis patients, per the 4D Study. Costs $150-$250 monthly. Side effects? Severe constipation for some.
- Lanthanum carbonate (Fosrenol): Also calcium-free. Often better tolerated than sevelamer. Price similar.
- Iron-based (ferric citrate, sucroferric oxyhydroxide): A two-for-one. Lowers phosphorus and boosts iron. Ferric citrate (Auryxia) costs $6,500-$7,200 a year. Expensive, but helpful if you’re anemic too.
Studies show sevelamer drops serum phosphorus by 1.2-1.8 mg/dL. That’s the difference between barely hitting target and staying safely below 5.5 mg/dL. But here’s the catch: 42% of patients quit phosphate binders within six months. Why? Cost. Side effects. The sheer number of pills. One Reddit user switched from sevelamer to lanthanum after constipation landed him in the ER. He paid $200 out-of-pocket-but it worked.
Current guidelines from KDIGO 2023 say: avoid calcium binders unless your calcium is below 9.5 mg/dL. Sevelamer or lanthanum are preferred. And if you’re on dialysis, iron-based binders are gaining ground.
Diuretics: Sweating Out the Fluid You Can’t Filter
Eighty to ninety percent of people with advanced kidney disease have fluid overload. Swollen ankles. Shortness of breath. High blood pressure that won’t budge. Diuretics are your body’s backup pump.
Loop diuretics like furosemide (Lasix), torsemide (Soaanz), and bumetanide are the go-to. They work on the loop of Henle in your kidneys, forcing out salt and water. Torsemide is stronger-30% more bioavailable than furosemide. A 20mg dose of torsemide equals 40mg of furosemide. And it lasts longer. That’s why 62% of patients in one survey preferred torsemide. It means fewer bathroom trips at night.
But here’s the problem: diuretic resistance. By stage 4 or 5 CKD, up to 60% of patients don’t respond well. Their kidneys just won’t pee enough. The fix? Add a thiazide diuretic like metolazone. It works lower down in the kidney. Together, they’re a powerful combo. But metolazone stops working if your eGFR drops below 30.
Cost-wise, generic furosemide is $4-$10 a month. Torsemide? $10-$25 for generic. Brand-name torsemide? $90-$120. The FIRST trial showed torsemide cut heart failure hospitalizations by 22% compared to furosemide. Yet most doctors still start with furosemide because it’s cheap and familiar.
Patients report the biggest issue isn’t side effects-it’s timing. Taking a diuretic at 8 a.m. means you’re running to the bathroom at 10 a.m., 1 p.m., and 3 p.m. Many split doses: half in the morning, half at noon. No afternoon doses. That’s what 65% of experienced users recommend to avoid sleep-killing midnight bathroom runs.

Anticoagulants: Preventing Clots When Your Blood Turns Sticky
People with kidney disease have a 2-4 times higher risk of stroke and heart attack. Why? Damaged kidneys trigger inflammation. Blood becomes thick. Clots form easily. If you have atrial fibrillation (AFib), your risk skyrockets.
Anticoagulants thin your blood to stop clots. But here’s the twist: your kidneys help clear most of these drugs. When kidney function drops, the drugs build up. Too much = bleeding. Too little = stroke.
Two main types:
- Warfarin (Coumadin): Old-school. Needs weekly INR blood tests. But it’s still the best choice if your eGFR is below 15 mL/min/1.73m². Why? We don’t have enough data on DOACs in severe kidney failure. Surprisingly, warfarin’s effect is more predictable in advanced CKD than DOACs, according to Dr. Jonathan Halperin.
- DOACs (apixaban, dabigatran, rivaroxaban, edoxaban): Newer, no blood tests needed. But dosing is tricky.
Apixaban (Eliquis) is the safest for CKD. In the ARISTOTLE trial, it cut major bleeding by 31% compared to warfarin in patients with eGFR 25-50. Dose? 2.5mg twice daily if your eGFR is 15-29. Annual cost: $6,200-$7,500.
Rivaroxaban (Xarelto)? Dose drops to 15mg daily if eGFR is 15-50. Edoxaban (Savaysa)? Contraindicated below eGFR 15.
Dabigatran (Pradaxa)? Reduces stroke risk by 34% over warfarin-but increases bleeding by 20% if eGFR is 30-50. Not ideal.
Current guidelines say: Use DOACs if your eGFR is 30 or higher. Apixaban is the top pick. If your eGFR drops below 30, switch to warfarin. If it’s below 15, warfarin is your only real option.
But here’s what patients say: One user on HealthUnlocked switched from apixaban to warfarin after unexplained bruising. “It meant weekly blood draws,” he wrote, “but at least I knew my level was safe.”
What Doctors Don’t Always Tell You
Medication errors are common in kidney disease. A JAMA Internal Medicine study found only 35% of primary care doctors dose anticoagulants correctly in CKD. Pharmacists? Better. Nephrologists? Best. But most patients see their PCP.
That’s why tools like the National Kidney Foundation’s “Medicines and CKD” app (downloaded 150,000 times) matter. It gives real-time dosing advice based on your eGFR. A Mayo Clinic study showed it cut medication errors by 27%.
Another hidden issue: phosphate binder adherence. Seventy percent of patients stop taking them within six months. Why? Too many pills. Stomach upset. Cost. The solution? Education. Take them WITH every bite of food-not before, not after. If you snack, take one. If you eat three meals and two snacks? That’s five doses a day. No exceptions.
Diuretic resistance? Add metolazone. But only if your eGFR is above 30. And never take it without your nephrologist’s OK.
And don’t assume newer = better. Ferric citrate costs $7,000 a year. Sevelamer? $2,000. Both work. Is the extra cost worth it? For some, yes. For others? Not if calcium acetate keeps phosphorus in range.

The Bigger Picture: What’s Changing in 2026
New drugs are coming. Tenapanor (Xphozah), approved in September 2023, blocks phosphate absorption differently than binders. It’s 30% more effective than sevelamer in trials. But it costs $6,800 a year. Will insurance cover it? Maybe not yet.
And SGLT2 inhibitors-like dapagliflozin-are now first-line for diabetic kidney disease. They reduce phosphorus naturally. Some patients who start these may never need phosphate binders.
The AUGUSTUS-CKD trial in early 2024 showed apixaban plus a single blood thinner (not two) cuts bleeding by 31% in CKD patients with AFib. That’s huge. Fewer bleeding events. Fewer hospital visits.
But the biggest challenge? Cost. One expert calls the average annual CKD medication bill $10,000+. “It’s unsustainable,” he says. The good news? Following current guidelines could save the U.S. healthcare system $12 billion a year by delaying dialysis and preventing heart attacks.
So what’s the takeaway? These medications aren’t just pills. They’re lifelines. But they’re only safe if you take them right, at the right dose, for your kidney function. Talk to your nephrologist. Use the app. Track your labs. Don’t skip doses because it’s expensive or inconvenient. Your heart and arteries are counting on it.
What to Ask Your Doctor
- What’s my current eGFR, and how does it affect my meds?
- Which phosphate binder is best for me-considering cost, side effects, and my calcium levels?
- Is torsemide a better fit than furosemide for my fluid overload?
- Should I be on apixaban, warfarin, or another anticoagulant? Why?
- Are there cheaper generic options that work just as well?
- Can I reduce my phosphate binder dose if I change my diet?

Post A Comment