Every year, more than 1.5 million people in the U.S. suffer harm from medication errors-many of which could have been stopped with a simple check. These aren’t rare mistakes. They happen in hospitals, pharmacies, and even at home when someone grabs the wrong pill bottle or misreads a label. The good news? Most of these errors are preventable. The key is knowing exactly what to look for: the medication name, the strength, and the dosage form. Get any one of these wrong, and the consequences can be deadly.
Why Checking Medication Details Isn’t Optional
It’s easy to assume that if a pill looks right, it must be right. But look-alike and sound-alike drug names cause thousands of errors every year. For example, prednisone and prednisolone sound nearly identical. One is for inflammation, the other for autoimmune conditions. Mix them up, and you could trigger serious side effects. Then there’s the infamous case of heparin: one vial contains 5,000 units per mL, another just 50 units per mL. A tenfold difference. One nurse in Sydney told me how she almost gave a patient the wrong one-until she paused, read the label again, and noticed the decimal placement.
Strength errors are even more common. A 2018 FDA report found that 34% of all medication errors involved incorrect strength. Why? Because people skip checking the numbers. They see “5 mg” on the prescription and assume the bottle says the same. But what if it says “50 mg”? Or worse-what if it says “5 mg” but the label is smudged, and the “0” looks like a “6”? That’s why you never rely on memory. Always compare the written order, the electronic record, and the physical medication-side by side.
Dosage form matters too. An oral tablet isn’t the same as a liquid, a patch, or an injection. Giving a capsule meant to be swallowed as a suppository can cause poisoning. Giving a topical cream as an eye drop? That’s a medical emergency. The dosage form tells you how the drug enters the body-and if you get it wrong, the drug may not work at all, or it could become dangerous.
The Three-Step Verification System
Healthcare professionals use a proven method called the “Three-Point Verification.” It’s simple, but it saves lives. You do it at three moments: when you receive the order, when you prepare the medication, and right before you give it to the patient.
- When you receive the order: Look for complete information. A safe prescription includes: drug name (full, no abbreviations), strength with units (e.g., “5 mg,” not “5mg”), dosage form (tablet, capsule, solution), route (oral, IV, topical), and frequency (once daily, every 6 hours). If any of these are missing, stop. Ask for clarification. Never guess.
- When you prepare the medication: Take the prescribed item and the physical medication out of the cabinet. Hold them side by side. Read the name aloud. Read the strength aloud. Read the dosage form aloud. Does the bottle match the order? If you’re using a pharmacy system, scan the barcode. If you’re in a hospital, use the barcode on the patient’s wristband and the medication. If the system doesn’t match, pause. Don’t proceed.
- Right before administration: Before you hand the medication to the patient, confirm their identity. Say their full name and date of birth. Then say out loud: “This is [drug name], [strength], [dosage form], for you. Is that correct?” Let them respond. This “read-back” method is used in 89% of successful error prevention stories reported by nurses.
This isn’t just for professionals. If you’re managing your own medications-or helping someone else-do this same check every single time you pick up a new prescription or refill.
What to Look for on the Label
Medication labels aren’t always clear. Some are crowded. Some use tiny fonts. Some still use dangerous abbreviations. Here’s what to scan for:
- Drug name: Always written in full. No “MS” for morphine sulfate (it could mean magnesium sulfate). No “U” for units (it looks like “0”). Always look for “unit” spelled out.
- Strength: Must have a space between number and unit. “10 mg” is correct. “10mg” is dangerous-it can be misread as “100 mg.” Also, never trust a decimal without a leading zero. “.5 mg” should be “0.5 mg.” Missing the zero can mean a tenfold overdose.
- Dosage form: Look for words like tablet, capsule, suspension, cream, patch, inhaler, or injection. If it’s missing, the label is incomplete. Don’t use it.
- Concentration: For liquids, check the ratio. “5 mg/mL” is clear. “1:10,000” is not. Epinephrine 1:10,000 should be written as “0.1 mg/mL.” The old format caused 236 errors between 2010 and 2015.
Also watch for “Tall Man” lettering-where part of the name is capitalized to highlight differences. PredniSONE vs. PredniSOLONE. That’s not a typo. It’s a safety feature.

Common Mistakes and How to Avoid Them
Even experienced staff slip up. Here are the most frequent errors-and how to stop them:
- Misreading “U” for “0”: Insulin doses are often written with “U” for units. But “10U” can look like “100.” Always write “units” in full. If you see “U,” ask for clarification.
- Confusing mcg and mg: Micrograms (mcg) are 1,000 times smaller than milligrams (mg). Giving 1 mg instead of 1 mcg of levothyroxine can cause a heart attack. Always spell out “micrograms” if possible. If you see “μg,” make sure it’s not a smudged “mg.”
- Assuming the pharmacy got it right: A 2020 study found that barcode scanning reduced dispensing errors by 83%. But if you skip the final check, you’re still at risk. Never assume automation is flawless. A 2021 study showed that 18% of errors happened because clinicians trusted the system too much.
- Ignoring high-alert medications: These are drugs that can cause serious harm if used wrong-insulin, heparin, opioids, IV potassium. They require double-checking by two trained staff members. If you’re at home, have someone else verify the label with you.
What Technology Can-and Can’t-Do
Electronic systems help. Epic and Cerner flag look-alike names. Barcode scanners catch mismatches. AI tools can now read labels with 99% accuracy. But technology isn’t magic. It can’t replace human attention.
One hospital in Melbourne found that after installing an AI label reader, nurses started skipping manual checks. Within six months, error rates rose again-not because the AI failed, but because people stopped thinking. The lesson? Use tech as a backup, not a replacement.
Also, not all systems are equal. Community pharmacies have lower adoption of verification tech than hospitals. If you’re picking up a prescription at a small pharmacy, don’t assume they have the same safeguards as a big hospital. Be your own safety net.
What You Can Do Right Now
You don’t need a medical degree to prevent a medication error. Here’s your action plan:
- Always ask for the full drug name, strength, and form when you get a new prescription.
- When you get the bottle, compare the label to the prescription slip or e-prescription on your phone.
- Read the strength out loud. Is it “5 mg” or “50 mg”? Is it “mcg” or “mg”?
- Check the form: Is it a tablet? A liquid? A patch? If it’s not what your doctor said, call the pharmacy.
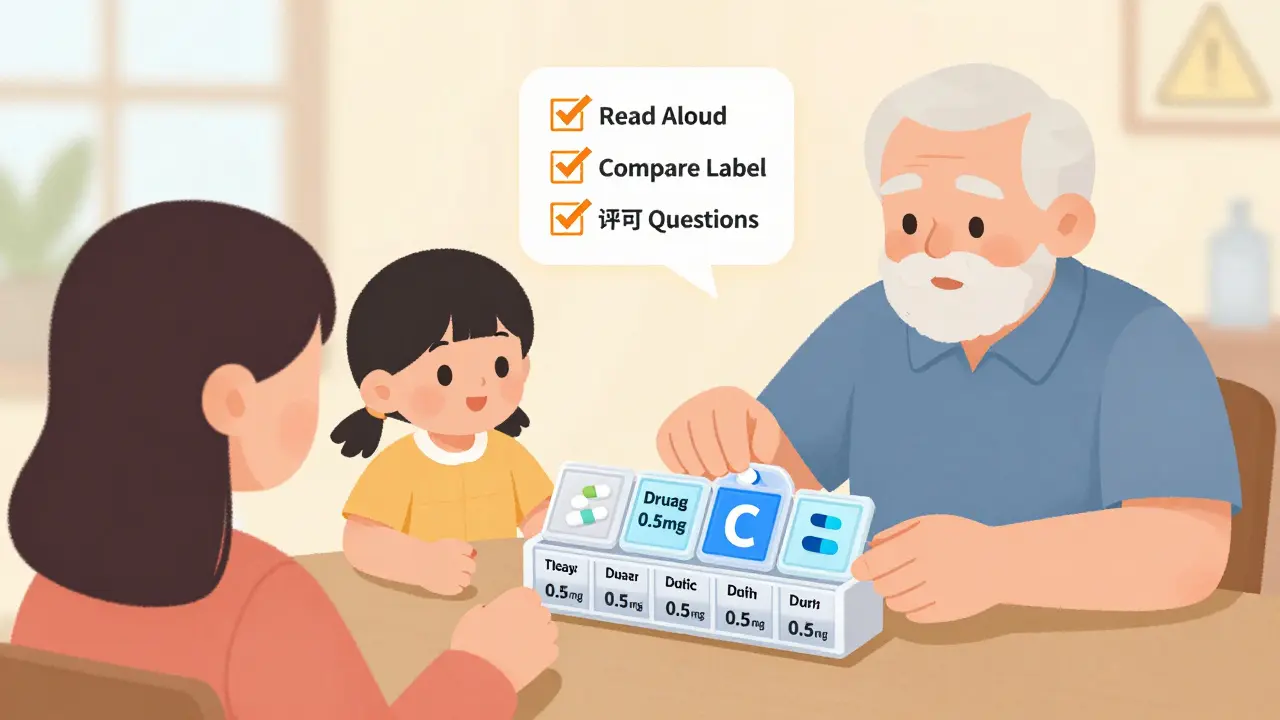
- Use a pill organizer with clear labels. Write the name, strength, and time on each compartment.
- If you’re helping an elderly parent or someone with memory issues, do the check with them every time they take a new pill.
It takes 30 seconds. But those 30 seconds could mean the difference between healing and harm.
Final Thought: Your Eyes Are Your Best Tool
Medication safety isn’t about fancy tech or complicated rules. It’s about slowing down. Looking closely. Reading everything. Saying it out loud. Asking questions. The system is designed to help-but it’s not perfect. And when it fails, you’re the last line of defense.
So next time you pick up a prescription, don’t just grab it and go. Stop. Look. Read. Verify. Because your life-or someone else’s-could depend on it.
What should I do if the medication label doesn’t match my prescription?
Stop. Do not take the medication. Call the pharmacy or prescriber immediately. Provide the exact details: drug name, strength, dosage form on the label, and what your prescription says. Never assume it’s a printing error. Many errors happen because people think, “It’s probably fine.” It’s not. Always verify.
Can I trust the pharmacy to catch mistakes?
Pharmacists are trained to catch errors, but they’re human-and they’re busy. A 2020 study showed that even with barcode systems, 1 in 100 prescriptions still has a mistake. That’s why you should always double-check yourself. Never rely on someone else to do your safety check. Your eyes and your questions are your best protection.
Why are spaces between numbers and units so important?
A space prevents misreading. “10mg” can be mistaken for “100 mg” if the “0” is smudged or unclear. “10 mg” makes it clear: the number is 10, the unit is mg. The Institute for Safe Medication Practices found that adding a space reduces unit misinterpretation errors by 12%. It’s a tiny change with a huge impact.
What abbreviations should I avoid on prescriptions?
Never trust these: “U” for units (use “units”), “mcg” instead of “μg” (μg can look like “mg”), “QD” for daily (use “daily”), “MS” for morphine sulfate (could mean magnesium sulfate), and “qd” or “q4h” (use “every day” or “every 4 hours”). The FDA and ISMP banned these abbreviations for good reason. If you see them, ask for clarification.
How do I know if a medication is a high-alert drug?
High-alert medications include insulin, heparin, opioids, IV potassium, and chemotherapy drugs. They’re often labeled as such in pharmacies and hospitals. If you’re unsure, ask the pharmacist: “Is this a high-alert medication?” If it is, insist on a second person verifying the dose-especially if you’re giving it at home. These drugs can cause serious harm even in small overdoses.
What if I’m helping an elderly relative who can’t read the label?
Create a simple chart: list each medication, its strength, dosage form, and time to take it. Use large print. Include a photo of the pill if possible. Keep it by the pill organizer. Check it every week. Call the pharmacy to confirm the label if anything looks off. Many older adults take 5+ medications-mistakes are common. Your attention can prevent a hospital visit.


Post A Comment