Graves’ disease isn’t just an overactive thyroid-it’s your immune system turning on itself. About 80% of all hyperthyroidism cases in the U.S. come from this single condition, where your body mistakenly attacks your thyroid gland, forcing it to pump out too much hormone. The result? Heart palpitations you can’t shake, weight loss even when you’re eating more, shaking hands, and sleepless nights. For many, it starts as just "feeling off"-until something breaks down completely.
What Happens When Your Immune System Attacks Your Thyroid
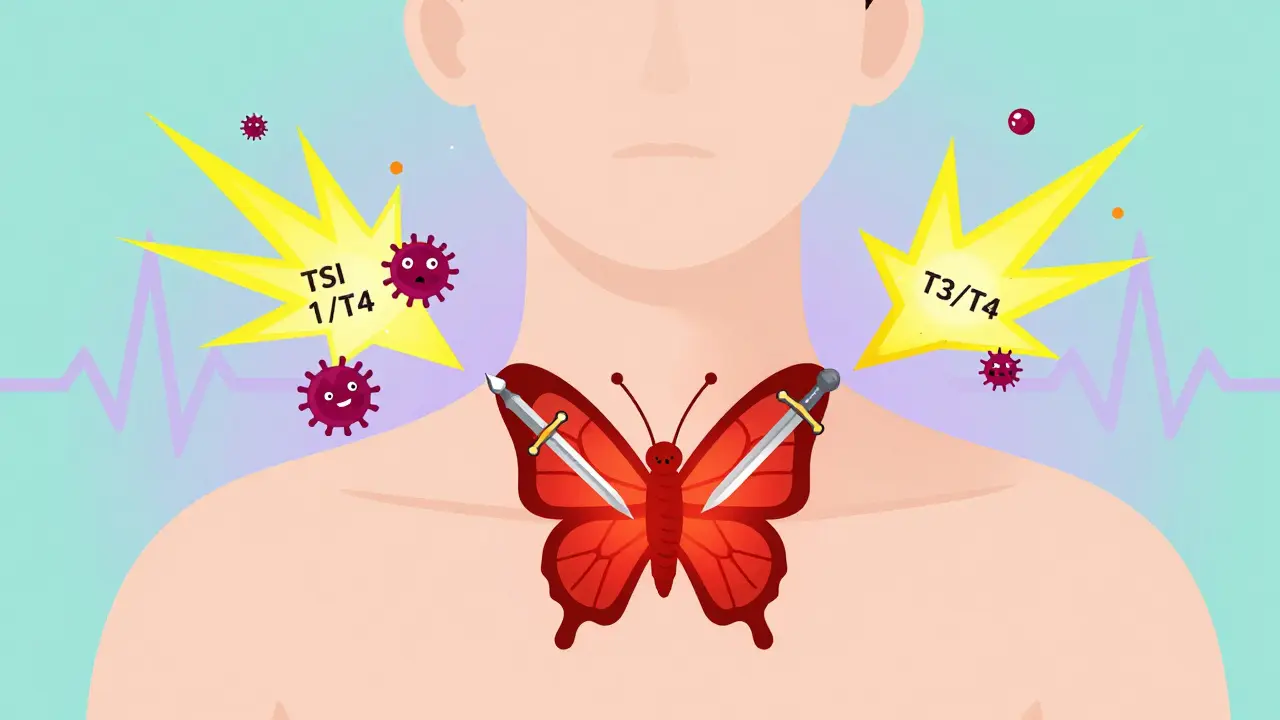
The thyroid sits like a butterfly at the base of your neck, quietly managing your metabolism, heart rate, and energy. In Graves’ disease, your immune system produces abnormal antibodies called thyroid-stimulating immunoglobulins (TSI). These don’t just float around-they latch onto your thyroid cells like keys in a lock, tricking the gland into thinking it needs to produce more hormones, even when it’s already overflowing.
This isn’t random. Women are seven times more likely to get it than men, especially between ages 30 and 50. If someone in your family has it, your risk jumps significantly-twin studies show genetics account for nearly 80% of susceptibility. Smoking doesn’t just hurt your lungs; it triples your chance of developing the eye complications tied to Graves’. And pregnancy? It can trigger it. About 5-10% of women develop symptoms within a year after giving birth.
The classic signs aren’t subtle. You might lose 15 to 20 pounds without trying, feel jittery even after coffee, have a racing heart, or notice your eyes bulging. About half of all patients develop Graves’ ophthalmopathy-swollen, red, or protruding eyes. In 3-5% of those cases, vision is at risk from nerve compression. A smaller group gets skin changes-thick, red patches on the shins or tops of feet, called pretibial myxedema. These aren’t side effects; they’re direct results of the same autoimmune attack.
How Doctors Diagnose Graves’ Disease
It’s not enough to just check your TSH. A low TSH (below 0.4 mIU/L) means your pituitary is trying to slow down your thyroid-but it’s not telling you why. That’s where free T4 and free T3 levels come in. In Graves’, free T4 is usually above 1.8 ng/dL and free T3 above 4.2 pg/mL. But the real clincher? Testing for TRAb, the thyroid-stimulating antibodies. These are present in 90-95% of Graves’ patients and are more accurate than any scan or ultrasound.
Many people wait months for a diagnosis because symptoms get mislabeled. On Reddit’s r/GravesDisease forum, 42% of users reported being told they had anxiety, depression, or menopause before getting the right answer. A 2023 survey found it took an average of 8 months to get diagnosed. That delay is dangerous. Left untreated, Graves’ disease increases your risk of heart failure and atrial fibrillation by 20-30%, according to the New England Journal of Medicine. In rare cases, it can trigger thyroid storm-a medical emergency with a 20-30% death rate.
Why PTU Is Still Used-Despite the Risks
There are three main ways to treat Graves’: antithyroid drugs, radioactive iodine, and surgery. Most adults start with methimazole-it’s taken once a day, works well, and has fewer serious side effects. But there’s one group where methimazole isn’t safe: pregnant women in their first trimester.
That’s where propylthiouracil (PTU) comes in. It crosses the placenta less than methimazole, lowering the risk of birth defects. For this reason, the American Thyroid Association still recommends PTU as the first-line drug during early pregnancy. But it’s not without cost. PTU carries a 0.2-0.5% risk of severe liver damage-sometimes fatal. The FDA requires a black box warning on every prescription. Patients on PTU need monthly liver function tests. One patient shared on HealthUnlocked: "PTU saved my pregnancy, but my ALT spiked to 120 U/L at week 24. I had to cut my dose in half. The fear never left me."
Other side effects are common too: 32% report a metallic taste or loss of appetite. About 18% say they get joint pain so bad it feels like arthritis. And while rare, agranulocytosis-a drop in white blood cells-can cause sudden fever or sore throat. If that happens, stop PTU immediately and go to the ER.
How PTU Compares to Other Treatments
| Treatment | Effectiveness | Side Effects | Cost (USD) | Long-Term Outcome |
|---|---|---|---|---|
| PTU | High (within weeks) | Liver toxicity (0.2-0.5%), taste changes, joint pain | $10-$30/month | 30-50% remission after 12-18 months; 40-60% relapse |
| Methimazole | High (slower than PTU) | Skin rash (0.1-0.3%), rare liver issues | $10-$50/month | Same remission rates as PTU |
| Radioactive Iodine (I-131) | 80-90% cure rate | Permanent hypothyroidism (50-80%), neck tenderness | $300-$1,500 | Lifelong thyroid hormone replacement needed |
| Thyroidectomy | 95% success | Voice changes (1%), low calcium (1-2%), scarring | $5,000-$15,000 | Permanent hypothyroidism |
Radioactive iodine is the most common long-term fix in the U.S., but it turns your thyroid into a non-functioning organ. You’ll need to take levothyroxine for life. Surgery removes the gland entirely-fast, definitive, but risky. PTU and methimazole are the only options that can actually put the disease into remission without destroying the thyroid.
Who Benefits Most from PTU?
PTU isn’t for everyone. It’s reserved for three specific cases: first-trimester pregnancy, severe thyroid storm (where rapid hormone suppression is critical), or when methimazole causes a severe allergic reaction. For non-pregnant adults, it’s a last resort.
But for pregnant women, it’s often the only choice. A 2023 study in Thyroid showed 75% of pregnant women on PTU reached normal hormone levels by the third trimester without harming the baby. Still, doctors monitor closely. Liver enzymes are checked every 4 weeks. The goal is to use the lowest possible dose and switch back to methimazole after the first trimester if safe.
For others, PTU might be used temporarily during thyroid storm-a life-threatening surge of thyroid hormones that causes fever, confusion, and heart failure. PTU works faster than methimazole here, blocking hormone release within hours. In those emergencies, it’s a bridge to stabilization.

What Happens After Treatment?
Even if your thyroid levels return to normal, the disease isn’t necessarily gone. About 30-50% of people achieve remission after 12-18 months of antithyroid drugs. But if you stop the medication, 40-60% will relapse within a year. That’s why doctors test TRAb levels again at 6 and 12 months after treatment. If they’re still high-above 10 IU/L-you’re at 80% risk of the disease coming back.
And even if your thyroid is calm, your eyes might not be. About 40% of patients continue to have eye symptoms after hormone levels normalize. Some need steroids, radiation, or even eye surgery. A new drug, teprotumumab, can reduce bulging eyes by 71%-but it costs $150,000 per course. Most insurance won’t cover it unless you’ve failed other treatments.
Living With Graves’ Disease: Real Challenges
It’s not just about pills and blood tests. The emotional toll is heavy. In a 2023 survey of 1,245 patients, 78% said anxiety and insomnia were their worst symptoms. Many felt like they were losing control of their bodies. Weight loss wasn’t a bonus-it was scary. Heart palpitations made them afraid to exercise. Sleepless nights turned into depression.
One woman in Sydney told her endocrinologist: "I stopped going out because I was shaking so badly in public. I thought I was having a panic attack. Turns out, it was my thyroid."
Support matters. The Graves’ Disease and Thyroid Foundation runs a 24/7 helpline, and online communities like Reddit’s r/GravesDisease have over 12,500 members sharing tips on managing fatigue, diet, and stress. Nutritionists often recommend avoiding excess iodine-seafood, kelp, iodized salt-because it can fuel the overactive thyroid.
The Future of Graves’ Disease Treatment
Research is moving fast. A new class of drugs called TSH receptor antagonists-like K1-70-is showing promise in trials. They block the antibody from binding to the thyroid without shutting down hormone production. That means no hypothyroidism. Phase 2 results showed 85% of patients returned to normal thyroid function.
Another breakthrough? B-cell depletion therapy with rituximab. In refractory cases, it triggered remission in 60% of patients. And the NIH has launched a $12.5 million Precision Medicine Initiative to predict who will respond to which treatment based on genetic markers like HLA-DR3.
For now, PTU remains a critical tool-not because it’s perfect, but because for some people, it’s the only thing that works without risking their baby or their life. It’s a balancing act: managing a dangerous drug to save a healthier future.

Post A Comment