Calcium & Vitamin D Calculator
Personalized Recommendations
Calcium Recommendations
Based on age, gender, and kidney function
Vitamin D Recommendations
Based on current vitamin D levels and kidney function
Quick Summary
- secondary hyperparathyroidism often stems from low calcium or vitamin D, especially in chronic kidney disease.
- Calcium and vitamin D work together to keep parathyroid hormone (PTH) in check.
- Targeted diet, supplements, and regular labs can prevent bone loss and cardiovascular risks.
- Vitamin D3 is generally more effective than D2 for raising serum levels.
- Monitoring serum calcium, phosphate, and PTH every 3-6 months guides safe treatment.
When the parathyroid glands start over‑producing hormone because of an external trigger, it’s called Secondary Hyperparathyroidisma condition where the body’s response to low calcium or vitamin D leads to excess parathyroid hormone. Most people link it to kidney disease, but the same hormonal surge can happen with poor nutrition, malabsorption, or certain medications. Understanding how Calciuma mineral vital for bone strength, muscle contraction, and nerve signaling and Vitamin Da fat‑soluble vitamin that helps the gut absorb calcium and regulates bone metabolism interact gives you practical tools to keep the glands calm and protect bone health.
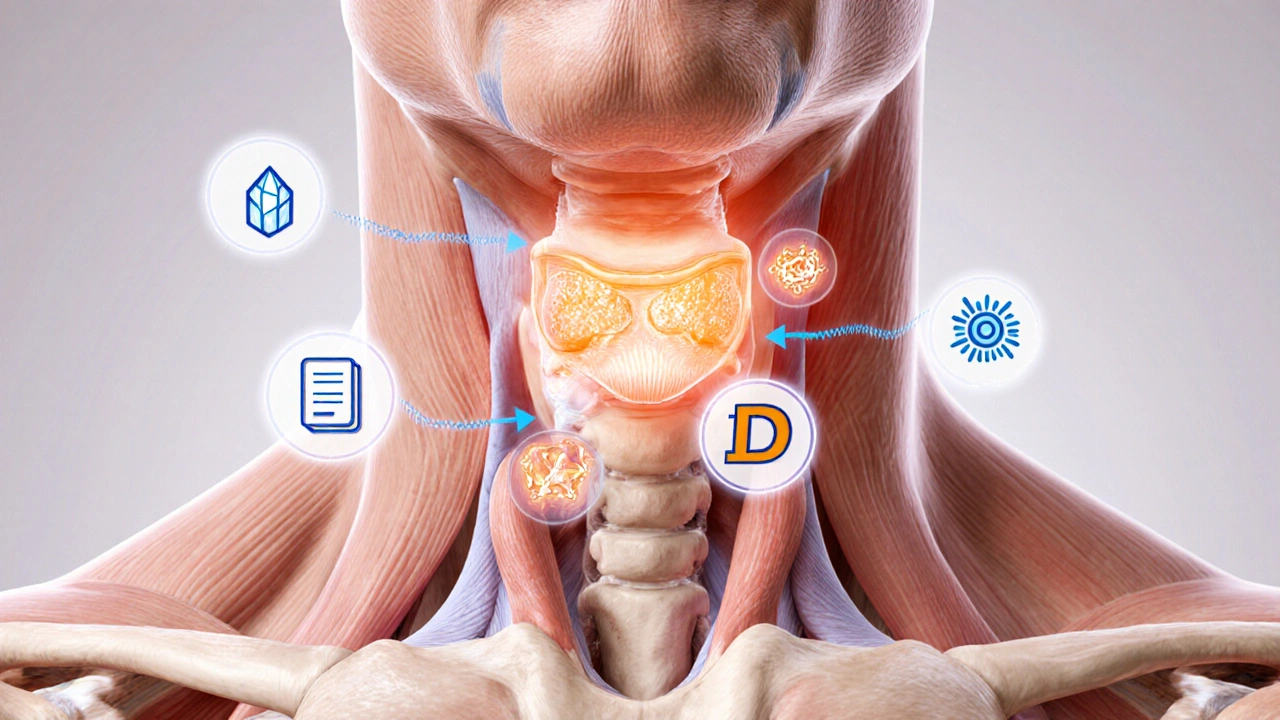
What Is Secondary Hyperparathyroidism?
The parathyroid glands sit behind the thyroid and release parathyroid hormone (PTH). PTH’s job is to raise blood calcium when it drops too low. In secondary hyperparathyroidism, the trigger - usually low calcium, low vitamin D, or high phosphate - forces the glands to work overtime. Over time, chronic elevation of PTH can erode bones, calcify blood vessels, and worsen kidney damage.
Key drivers include:
- Chronic kidney disease (CKD), where the kidneys can’t convert vitamin D to its active form.
- Dietary calcium deficiency or malabsorption syndromes.
- Vitamin D insufficiency from limited sunlight or poor intake.
- Use of certain anti‑seizure meds that increase phosphate.
Understanding the loop helps you break it: raise the serum calcium enough to signal the glands to quit over‑producing PTH.
How Calcium Helps Keep PTH in Check
Calcium is the most abundant mineral in the body, stored mostly in bones. When blood calcium dips, PTH swoops in, pulling calcium from bone, increasing kidney reabsorption, and prompting the gut to absorb more (via vitamin D activation). By maintaining a steady dietary calcium intake, you give the body a reason not to crank up PTH.
Practical tips:
- Aim for 1,000mg of calcium daily if you’re under 50, and 1,200mg if you’re older.
- Choose dairy (milk, yogurt, cheese) or fortified plant milks when dairy isn’t an option.
- Include low‑oxalate leafy greens like bokchoy and kale, which provide calcium without inhibiting absorption.
When you consistently hit these targets, most people see a modest 10‑15% drop in PTH within weeks.

Vitamin D’s Role in the Calcium‑PTH Equation
Vitamin D exists as D2 (ergocalciferol) and D3 (cholecalciferol). Both turn into 25‑hydroxyvitamin D in the liver, then into the active hormone 1,25‑dihydroxyvitamin D in the kidneys. This active form tells the intestines to absorb calcium and phosphate.
Insufficient vitamin D means the gut can’t grab enough calcium, even if you eat plenty. The body reacts by releasing more PTH - the classic secondary hyperparathyroidism loop.
Key facts:
- Serum 25‑OH‑vitamin D < 20ng/mL is considered deficient.
- Levels between 20‑30ng/mL are insufficient and may already trigger hormonal changes.
- Optimal range for most adults is 30‑50ng/mL, especially if you have CKD.
Because the kidneys convert vitamin D to its active form, patients with CKD often need the active form (calcitriol) or analogs to bypass the defective step.
Calcium + Vitamin D: The Perfect Pair
Think of calcium as the brick and vitamin D as the mortar. Without enough mortar, bricks won’t stick together, and the structure collapses. Supplementing calcium alone can raise serum calcium slightly, but without vitamin D the gut absorption stays low, limiting the benefit.
Clinical guidelines (KDIGO 2023) recommend combining calcium (500‑1000mg) with vitamin D (800‑1,000IU of D3) for CKD stages3‑5 not on dialysis. The combo reduces PTH by 20‑30% on average.
When you start a supplement plan, monitor these labs every 3months:
- Serum Calciumthe amount of calcium circulating in the blood
- Serum Phosphatephosphate levels that rise when kidneys can’t excrete it
- Parathyroid Hormone (PTH)the hormone that rises in response to low calcium
If calcium goes too high (>10.5mg/dL), you risk vascular calcification, especially in kidney disease. That’s why balance, not excess, is key.
VitaminD2 vsVitaminD3: Which Is Better?
| Attribute | Vitamin D2 (Ergocalciferol) | Vitamin D3 (Cholecalciferol) |
|---|---|---|
| Source | Plants, fortified foods | Animal‑based foods, sunlight‑derived |
| Potency | ~70% of D3 potency | Reference standard |
| Half‑life | ~15 days | ~22 days |
| Rise in 25‑OH‑vitaminD | Modest increase | More robust increase |
| Preferred for CKD patients | Less common | Generally recommended |
Because D3 raises blood levels faster and stays active longer, most clinicians prescribe it unless a strict vegan regimen is required.

Lifestyle Tips to Support Calcium & VitaminD
Beyond pills, everyday habits make a big difference:
- Sun exposure: 10‑15minutes of midday sun on face and arms, 2‑3 times a week, can supply 1,000‑2,000IU of D3.
- Limit phosphate additives: Processed meats, colas, and some baked goods contain hidden phosphate that drives PTH up.
- Stay active: Weight‑bearing exercise (walking, resistance training) stimulates bone formation and improves calcium utilization.
- Avoid high‑dose calcium without vitamin D: Large calcium loads (e.g., 2,000mg in one go) can cause kidney stones.
Medical Management and When to See a Doctor
If labs show PTH above 70pg/mL with low calcium or vitamin D, you’re likely in secondary hyperparathyroidism territory. Here’s what doctors typically do:
- Correct vitamin D deficiency first - give a loading dose of 50,000IU weekly for 8weeks, then maintenance 1,000‑2,000IU daily.
- Introduce calcium carbonate or calcium citrate (500‑1,000mg) split into two doses with meals.
- For CKD patients, add active vitamin D analogs (calcitriol) or phosphate binders if serum phosphate stays high.
- Re‑check labs after 6-12weeks; adjust doses to keep calcium 8.5‑10.2mg/dL, phosphate 2.5‑4.5mg/dL, and PTH trending down.
Rarely, severe resistant cases need surgical removal of part of the parathyroid glands (parathyroidectomy). That’s a last resort after medical therapy fails.
Common Pitfalls & How to Avoid Them
- Over‑supplementing calcium: More isn’t always better; excess can precipitate vascular calcification.
- Ignoring phosphate: Low calcium plus high phosphate fuels PTH; binders like sevelamer help.
- Skipping follow‑up labs: Hormone levels swing quickly; without monitoring you may over‑correct.
- Relying on single‑source vitamin D: Sun, diet, and supplements should all be considered.
Frequently Asked Questions
Can I treat secondary hyperparathyroidism with diet alone?
Diet helps, but most people need supplements. Raising 25‑OH‑vitaminD above 30ng/mL and meeting calcium goals usually lowers PTH enough to avoid medication, especially in early CKD.
What’s the safe upper limit for calcium intake?
The tolerable upper intake for adults is about 2,500mg per day. Going over this consistently raises the risk of kidney stones and arterial calcification.
Is vitaminD3 safe for people with kidney disease?
Yes, but dosage may need adjustment. In advanced CKD the kidneys can’t activate D3, so doctors often prescribe active forms like calcitriol instead.
How often should I get my labs checked?
Every 3‑6months if you’re on supplements, and more frequently (monthly) if you’re on active vitaminD analogs or have rapidly changing kidney function.
Can high phosphate foods worsen secondary hyperparathyroidism?
Yes. Foods like processed cheese, sodas, and certain meats add phosphate that the kidneys struggle to clear, pushing PTH higher.
Bottom line: keeping your calcium and vitaminD in the right range stops the parathyroid glands from over‑reacting, shields your bones, and lowers the cardiovascular risk that comes with secondary hyperparathyroidism. Start with a balanced diet, add supplements if labs say you need them, and keep an eye on the numbers. If you’re unsure, a quick chat with your GP or nephrologist can set you on the right path.

Post A Comment