Antipsychotic Comparison for Parkinson's Disease
This tool helps patients and caregivers understand the critical differences between antipsychotics when treating psychosis in Parkinson's disease. Based on the article's discussion of dopamine mechanisms, the table below shows which medications are safer for Parkinson's patients and why.
How to Interpret This Comparison
| Antipsychotic | Motor Risk Level | Psychosis Effectiveness | FDA Approved for PD | Cost/Access | Key Considerations |
|---|---|---|---|---|---|
| Pimavanserin (Nuplazid) | Low | High (45-50% reduction in psychosis) | Yes | High ($434M sales) Limited insurance coverage |
Works on serotonin receptors (not dopamine), so no motor worsening. Only FDA-approved specifically for Parkinson's psychosis. |
| Quetiapine | Moderate | Moderate (30-40% reduction) | Off-label | Moderate Generic available |
Dopamine-sparing but still affects movement in ~50% of patients. Requires cautious dosing. |
| Clozapine | Moderate | High (50-60% reduction) | Off-label | Moderate Requires blood monitoring |
Very effective for psychosis but requires regular blood tests. Dopamine-sparing but still has some motor risk. |
| Haloperidol | High | Moderate (35-45% reduction) | No | Low |
Strong dopamine blocker that severely worsens motor symptoms (25-35% decline). Should be avoided in Parkinson's. |
| Risperidone | High | Moderate (30-40% reduction) | No | Low |
Significant motor worsening (25-35%), especially in early Parkinson's. Often causes rapid decline in mobility. |
| Olanzapine | High | Moderate (35-40% reduction) | No | Low |
High risk of motor worsening (30-35%) and sedation. Often leads to significant mobility issues. |
Important Note
The article emphasizes that even when using the safest options like pimavanserin, patients need regular monitoring. Only 42% of specialists prescribe pimavanserin due to cost and access issues. Always consult a movement disorder specialist for personalized treatment.
When someone with Parkinson’s disease starts having hallucinations or delusions, doctors face a brutal choice: treat the psychosis and risk making their tremors worse, or leave the psychosis untreated and watch their quality of life crumble. The reason this dilemma exists isn’t complicated-it’s levodopa and antipsychotics working in opposite directions on the same brain chemical: dopamine.
How Levodopa Works (and Why It’s a Double-Edged Sword)
Levodopa is the gold standard for treating Parkinson’s. It’s not a drug that directly gives you dopamine-it’s a building block. Your brain converts it into dopamine, especially in the parts that have lost dopamine-producing cells. That’s why it helps with stiffness, slowness, and shaking. But here’s the catch: as Parkinson’s gets worse, the brain loses its ability to control how much dopamine gets released. What used to be a steady trickle becomes a flood. A single dose of levodopa can spike dopamine levels way beyond what’s normal, especially in the later stages. This isn’t just inefficient-it’s unstable. And that instability makes the brain hypersensitive to anything that tries to block dopamine.
How Antipsychotics Work (and Why They’re Dangerous in Parkinson’s)
Antipsychotics like haloperidol, risperidone, and olanzapine were designed to calm overactive dopamine signaling in schizophrenia. They do this by sticking to dopamine D2 receptors and blocking them-like putting a lock on a door so dopamine can’t get in. For someone with psychosis, that’s helpful. But in Parkinson’s, those same receptors are already starved for dopamine. Blocking them doesn’t just reduce hallucinations-it makes movement even harder. Studies show that even low doses of these drugs can make motor symptoms worse by 25% to 35% on standard rating scales. That means someone who could walk with a cane might suddenly need a wheelchair after starting an antipsychotic.
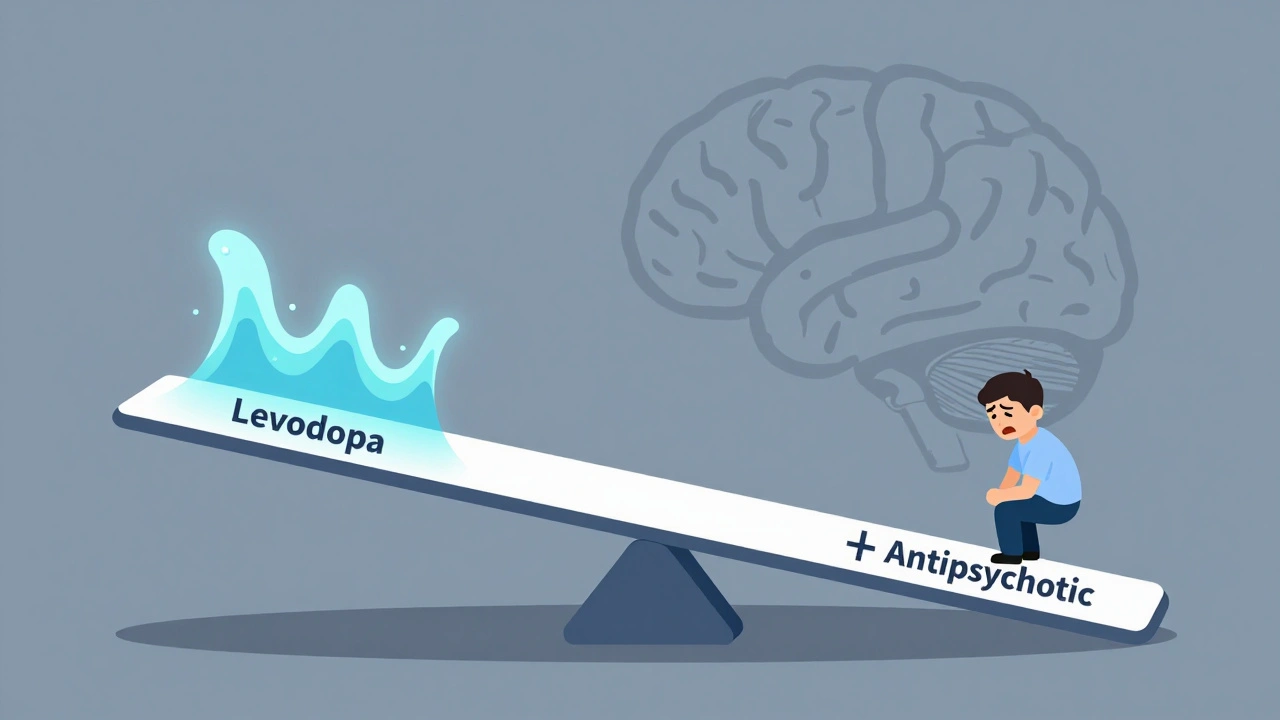
The Perfect Storm: When Both Drugs Are Used Together
Imagine a seesaw. On one side is levodopa, pushing dopamine levels up. On the other side is an antipsychotic, trying to push dopamine signaling down. In a healthy brain, this balance is easy to maintain. In a Parkinson’s brain, it’s impossible. The result? A patient might get slightly less hallucinating-but now they can’t get out of bed. Or, if the antipsychotic is stopped suddenly, dopamine surges can trigger a rare but deadly condition called neuroleptic malignant syndrome (NMS), with symptoms like high fever, muscle rigidity, and confusion. Mortality rates for NMS range from 10% to 20%. This isn’t theoretical. At the Cleveland Clinic, case reports from 2021 to 2023 show 17 Parkinson’s patients who went from mild symptoms to severe disability within 72 hours of starting a low-dose antipsychotic.

What About Schizophrenia Patients Who Need Levodopa?
This isn’t just a Parkinson’s problem. Sometimes, people with schizophrenia develop Parkinson-like symptoms from long-term antipsychotic use. Doctors might consider levodopa to help with stiffness or tremors. But here’s the twist: giving levodopa to someone with schizophrenia can trigger a psychotic relapse. A 1988 study found that 60% of schizophrenia patients given just 300 mg of levodopa had their hallucinations and delusions return-sometimes worse than before. Even if they’d been stable for years. That’s because levodopa doesn’t just boost dopamine where it’s needed-it floods areas already overactive. It’s like turning up the volume on a noisy room instead of turning off the speaker.
There Are Exceptions-But They’re Narrow
Not all antipsychotics are created equal. Quetiapine and clozapine are considered “dopamine-sparing,” meaning they don’t block D2 receptors as strongly. That’s why quetiapine is sometimes used in Parkinson’s psychosis-though even then, about half of patients still see some motor worsening. Pimavanserin is different. It doesn’t touch dopamine at all. Instead, it works on serotonin receptors. Approved in 2016 specifically for Parkinson’s psychosis, it’s the only antipsychotic that doesn’t make movement worse. But it’s expensive-$434 million in sales in 2022-and not everyone has access to it. And even pimavanserin doesn’t fix the root problem. It just sidesteps it.
What Clinicians Are Doing About It
Most movement disorder specialists avoid typical antipsychotics entirely. A 2022 survey of 150 specialists found that 89% won’t use haloperidol or risperidone in Parkinson’s patients. Only 42% have prescribed pimavanserin, mostly because of cost and insurance hurdles. The rest rely on non-drug strategies: reducing other medications that worsen psychosis, improving sleep, lowering lighting to reduce visual distortions, and treating infections or dehydration that can trigger confusion. For those who need medication, the rule is simple: start low, go slow, and monitor daily. The Cleveland Clinic requires daily motor assessments for the first two weeks after starting any antipsychotic. If a patient’s UPDRS score (a standard Parkinson’s rating) goes up by more than 15 points, the drug is stopped immediately.
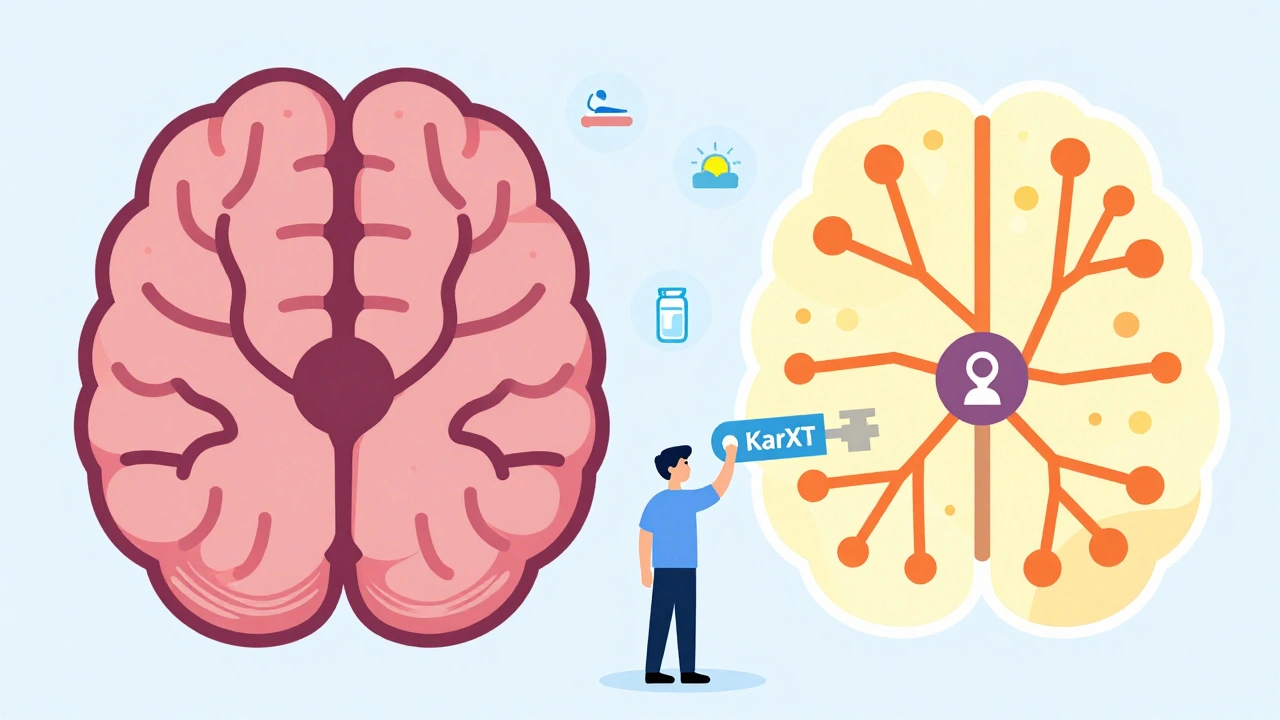
The Future: New Drugs That Don’t Touch Dopamine
Researchers are tired of playing whack-a-mole with dopamine. The next wave of treatments targets other brain systems. KarXT, a combination drug that acts on muscarinic receptors, showed in a 2023 trial that it reduced psychosis in Parkinson’s patients without worsening movement at all. That’s huge. Other drugs targeting serotonin and acetylcholine are in development. The FDA now explicitly asks drug companies to prove their new psychosis treatments won’t hurt motor function. Meanwhile, the Parkinson’s Progression Markers Initiative is using brain scans to predict who’s most at risk. If a patient’s dopamine transporter scan shows very low levels, they’re 80% more likely to have severe motor worsening if given an antipsychotic. That kind of precision could change everything.
What Patients and Families Should Know
If you or a loved one has Parkinson’s and is experiencing hallucinations, don’t assume antipsychotics are the only answer. Talk to a movement disorder specialist-not just a general neurologist. Only 38% of general neurologists feel confident managing this issue. Ask about pimavanserin, even if it’s expensive. Ask about non-drug strategies. And never stop or start these medications without medical supervision. Abruptly stopping levodopa can trigger NMS. Abruptly stopping an antipsychotic can cause rebound psychosis. The balance is fragile, and the stakes are high.
Why This Matters Beyond the Clinic
Over 1 million Americans with Parkinson’s develop psychosis. Yet 65% of them get no specific treatment because doctors fear making their movement worse. That’s not just a medical problem-it’s a quality-of-life crisis. People stop leaving the house. They stop eating. They stop talking. The market for better treatments is growing fast-projected to hit $2.3 billion by 2027. But money alone won’t fix this. What’s needed is a shift in thinking: psychosis in Parkinson’s isn’t just a psychiatric issue. It’s a neurological one. And treating it requires understanding the brain’s chemistry, not just its symptoms.
Can levodopa make psychosis worse in Parkinson’s patients?
Yes. While levodopa is essential for movement, it can worsen hallucinations and delusions in 15% to 20% of Parkinson’s patients, especially at higher doses or in advanced disease. This happens because levodopa increases dopamine in brain areas already prone to overactivity, triggering or intensifying psychotic symptoms.
Why can’t doctors just use any antipsychotic for Parkinson’s psychosis?
Most antipsychotics block dopamine D2 receptors, which are already under-stimulated in Parkinson’s. Blocking them further makes stiffness, slowness, and tremors significantly worse-sometimes severely. Even low doses of drugs like risperidone or haloperidol can cause sudden, dramatic motor decline within days.
Is there an antipsychotic that doesn’t worsen Parkinson’s symptoms?
Yes-pimavanserin (Nuplazid). It works by targeting serotonin receptors instead of dopamine, so it doesn’t interfere with movement. It’s FDA-approved specifically for Parkinson’s psychosis. However, it’s expensive and not always covered by insurance. Other options like quetiapine are used cautiously, but even these can cause some motor worsening in up to half of patients.
What happens if you suddenly stop taking an antipsychotic in someone with Parkinson’s?
Stopping antipsychotics abruptly can trigger neuroleptic malignant syndrome (NMS), a life-threatening condition with high fever, muscle rigidity, confusion, and organ failure. It’s rare-occurring in 0.01% to 0.02% of cases-but the mortality rate is 10% to 20%. Always taper off under medical supervision.
Are there new treatments coming for Parkinson’s psychosis?
Yes. KarXT, a new drug targeting muscarinic receptors, showed in a 2023 trial that it reduced psychosis without worsening motor symptoms. Other drugs targeting serotonin and acetylcholine are in development. Researchers are also using brain scans to predict who will respond poorly to antipsychotics, allowing for personalized treatment plans.

Post A Comment