What Exactly Is Statin Intolerance?
Statin intolerance isn’t just about feeling sore after taking a cholesterol pill. It’s when your body reacts badly enough to make you stop taking a drug that could save your life. Around 7% to 29% of people on statins report muscle pain, weakness, or cramps. But here’s the catch: only 5% to 15% of those cases are truly caused by the statin. Most of the time, something else is to blame-low vitamin D, an underactive thyroid, or even just aging muscles.
The problem? Many patients get labeled as "statin intolerant" and quit the medication for good. That’s dangerous. Statins lower LDL (bad) cholesterol by 30% to 50%, and every 1 mmol/L drop reduces your risk of heart attack or stroke by 20% to 25%. For someone with high cholesterol and a history of heart disease, walking away from statins is like refusing a seatbelt in a speeding car.
Why Most Clinics Get It Wrong
Traditional doctors often don’t have the time or tools to dig deeper. A patient says, "My legs hurt since I started simvastatin," and the doctor says, "Stop it." No tests. No follow-up. No attempt to find a solution. That’s why 45% of patients who report muscle symptoms end up permanently off statins-even though most could tolerate them with the right approach.
Specialized statin intolerance clinics change that. They don’t just stop the drug. They investigate. They test. They rechallenge. They switch. They adjust. And they get results. At Cleveland Clinic, for example, 68% of patients who walked in saying they couldn’t take statins ended up back on some form of lipid-lowering therapy after following their protocol.
The Four-Step Protocol That Works
Here’s what a real statin intolerance clinic does, step by step:
- Stop the statin for two full weeks. No exceptions. Symptoms should begin to fade within days. If they don’t, the problem isn’t the statin.
- Rule out other causes. Check thyroid function, vitamin D levels, kidney and liver health, and review all supplements (like red yeast rice or CoQ10). Some drugs-like fibrates or certain antibiotics-can make muscle symptoms worse when mixed with statins.
- Rechallenge with a different statin. Don’t try the same one again. Switch from a lipophilic statin (like simvastatin or atorvastatin) to a hydrophilic one (like rosuvastatin or pravastatin). Hydrophilic statins stay mostly in the liver, not the muscles, making them far less likely to cause pain.
- Try intermittent dosing. If daily dosing still causes issues, switch to every other day or twice a week. Rosuvastatin, with its long half-life, works well for this. Studies show 76% of patients who failed daily statins tolerate this approach and still get their LDL down by 20% to 40%.
When Statins Just Won’t Work: What Comes Next?
Some people truly can’t take any statin-even at low doses or on alternate days. That’s where non-statin options come in. The first-line choice? Ezetimibe. It’s cheap-about $35 a month-and proven to cut heart events by 6% when added to lifestyle changes. It doesn’t cause muscle pain. It’s gentle. And it works.
If ezetimibe isn’t enough, bempedoic acid (Nexletol) is the next step. Approved in 2020, it lowers LDL by about 18% and has almost no muscle-related side effects. Unlike statins, it’s activated only in the liver, not in muscle tissue. That’s why the CLEAR Outcomes trial with over 14,000 patients showed no increase in muscle complaints.
PCSK9 inhibitors like evolocumab are powerful-they slash LDL by 60%-but they cost over $5,800 a year. Insurance often denies them unless you’ve tried everything else. That’s why clinics use them as a last resort, not a first.
What Patients Say About These Clinics
"I was told I was statin intolerant for five years," says a Reddit user named HeartPatient87. "Then I went to Johns Hopkins. They put me on rosuvastatin 5mg twice a week with CoQ10. My LDL dropped from 142 to 89. No pain. No fatigue. I finally feel like I’m in control."
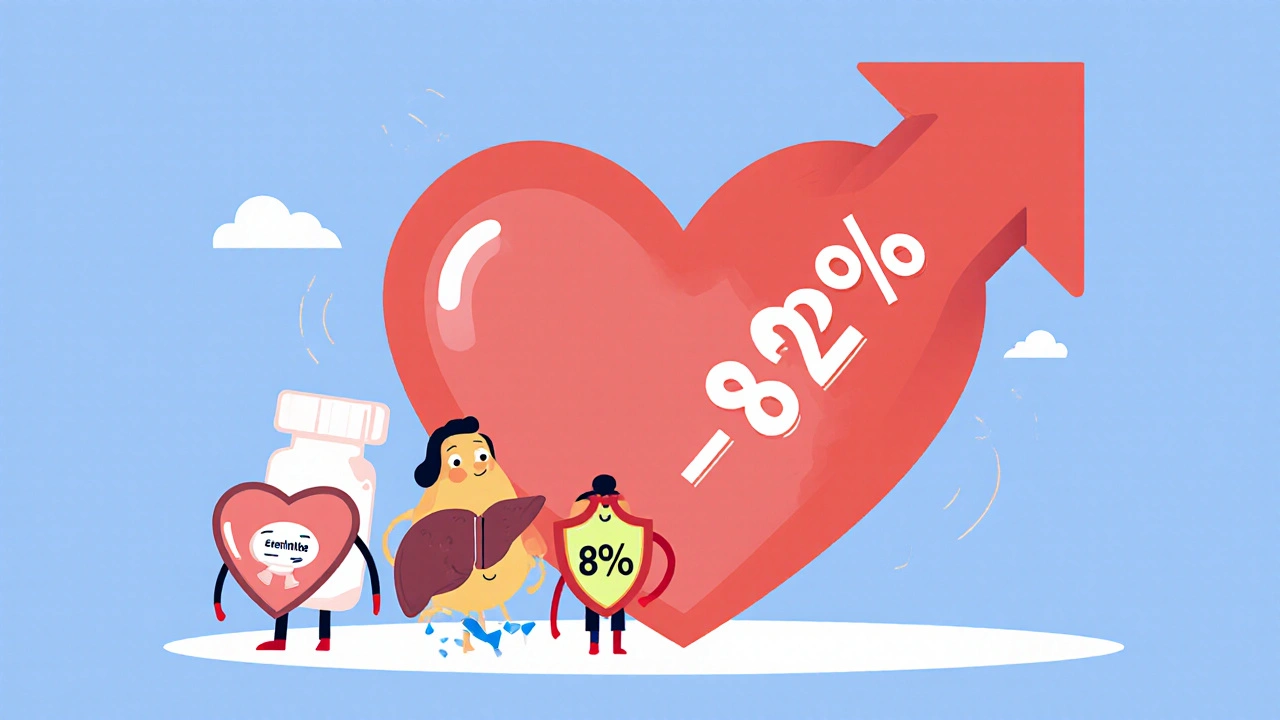
At Kaiser Permanente, 82% of patients in their statin intolerance program were able to resume some form of cholesterol-lowering therapy. Compare that to 45% in regular clinics. The difference? Structure. Follow-up. Testing. Personalization.
But it’s not perfect. Many patients complain about long wait times-6 to 8 weeks to see a lipid specialist. Others fight insurance companies for months just to get access to bempedoic acid or PCSK9 inhibitors. One patient on Inspire shared: "I met all the criteria for PCSK9 inhibitors. My insurance denied it four times. Took 11 weeks of appeals."
Who Benefits Most From These Clinics?
These protocols aren’t just for people with mild muscle aches. They’re essential for:
- People with a history of heart attack or stroke
- Diabetics with high LDL
- Those with familial hypercholesterolemia
- Patients who’ve had a stent or bypass surgery
For these people, not lowering LDL isn’t an option. The goal isn’t to avoid side effects at all costs-it’s to find a way to lower cholesterol that works for their body. That’s what these clinics do.
What’s New in 2025?
Things are moving fast. Mayo Clinic started genetic testing in 2023 for the SLCO1B1 gene variant, which makes some people more prone to simvastatin muscle damage. If you carry it, you avoid simvastatin entirely.
Researchers are also testing nanoparticle statins-tiny drug carriers that deliver the medicine directly to the liver. Early trials show 92% of patients tolerate them without muscle pain. Phase 2 results are promising, and if approved, they could change everything.
Intermittent dosing is now the go-to strategy for 78% of lipid specialists surveyed in 2024. It’s safe, effective, and affordable. And it’s finally getting the attention it deserves.
Why This Matters More Than Ever
Over 39 million Americans take statins. Between 2.7 and 11.3 million of them might be mislabeled as intolerant. That’s millions of people walking around with untreated high cholesterol, unaware that there’s a way back on medication that won’t hurt them.
Statin intolerance clinics aren’t luxury services. They’re medical necessity. They turn dead ends into pathways. They prevent heart attacks by fixing what broken protocols broke.
And the data doesn’t lie: structured, step-by-step care leads to better outcomes, fewer hospitalizations, and longer lives.
What You Can Do Today
If you’ve been told you’re statin intolerant:
- Don’t assume it’s permanent.
- Ask for a referral to a lipid specialist or a statin intolerance clinic.
- Request a full workup: thyroid, vitamin D, CK levels, drug interactions.
- Ask about switching to rosuvastatin or pravastatin.
- Ask if intermittent dosing is an option.
- Ask about ezetimibe or bempedoic acid if statins still don’t work.
There’s no shame in needing help. Statins aren’t one-size-fits-all. And no one should be forced to choose between their heart and their muscles.


Post A Comment