DVT Psychological Impact Assessment
Receiving a DVT diagnosis can trigger various emotional reactions. This tool helps you recognize common psychological impacts and learn effective coping strategies.
Anxiety
Persistent worry, heart-racing, difficulty sleeping.
Typical onset: Hours to daysDepression
Low mood, loss of interest, fatigue.
Typical onset: Weeks after diagnosisHealth-Related PTSD
Flashbacks, avoidance of medical care, hyper-vigilance.
Typical onset: Months, especially after complicationsCoping Strategies
- Ask for a Simple Explanation: Request that your provider describe the clot, its location, and the treatment plan in plain language.
- Schedule a Mental-Health Check: Many vascular clinics screen for anxiety or depression during the first visit.
- Use Mind-Body Techniques: Guided breathing, progressive muscle relaxation, or mindfulness apps help lower short-term anxiety.
- Stay Physically Active Within Limits: Light walking, ankle pumps, and compression stockings improve circulation and boost mood.
- Connect with Others: Join a patient support group online or in-person to share experiences and encouragement.
- Track Your Thoughts: Journaling about fears helps identify patterns and reframe irrational beliefs.
- Limit Over-Research: Pick reputable sources like the American Heart Association to avoid health anxiety.
Healthcare Provider Best Practices
- Deliver the diagnosis in a private, calm setting.
- Use lay terms and check for understanding.
- Offer written summaries covering both medical and emotional coping tips.
- Screen for anxiety, depression, and PTSD using tools like GAD-7 or PHQ-9.
- Refer patients to mental-health professionals when needed.
- Schedule a follow-up call within a week to address lingering worries.
Resources for Support
- National Blood Clot Alliance (NBCA): Printable guides, webinars, and moderated forums.
- American Psychological Association (APA) – Find a Therapist: Search by specialty in health anxiety or chronic illness coping.
- Local Hospital Social Work Departments: Free counseling sessions for recent diagnoses.
- Mobile Apps: “Calm” and “Headspace” offer modules for medical anxiety.
- Physical Therapy Clinics: Safe, clot-friendly activity plans to keep you moving.
When to Seek Immediate Help
- Sudden shortness of breath, chest pain, or coughing up blood—possible pulmonary embolism.
- Severe, unrelenting anxiety leading to panic attacks and inability to function.
- Thoughts of self-harm or hopelessness—contact a crisis line immediately.
Quick medical attention prevents physical complications and opens doors for urgent mental-health support.
Receiving a diagnosis of deep vein thrombosis can feel like the ground just dropped out from under you. Beyond the physical risks, the news often triggers a storm of thoughts, fears, and emotions that linger long after the clot is treated.
Key Takeaways
- Emotional reactions to a DVT diagnosis are common and can include anxiety, depression, and health‑related PTSD.
- Factors such as personal medical history, support networks, and how information is delivered shape the psychological impact.
- Early screening for mental distress and timely referrals to mental‑health professionals improve outcomes.
- Practical coping tools-mindfulness, activity modification, and patient support groups-help restore confidence.
- Healthcare providers play a crucial role by delivering clear explanations and integrating mental‑health care into treatment plans.
What is Deep Vein Thrombosis?
When doctors confirm deep vein thrombosis is a blood clot forming in the deep veins, typically in the legs, that can obstruct blood flow and pose serious health risks, the immediate concern is physical-preventing the clot from traveling to the lungs and causing a pulmonary embolism. However, the diagnosis also introduces a psychological dimension that many patients overlook.
Typical Emotional Reactions
Most patients report an instant surge of fear. The word “clot” conjures thoughts of heart attacks and sudden death, even though the medical reality differs. This fear often morphs into anxiety, characterized by racing thoughts about future health, work ability, and family responsibilities.
In parallel, feelings of loss of control emerge. Suddenly, a routine activity like a long flight or a day at the office feels risky. Such loss can trigger depressive moods, where motivation dips, sleep patterns shift, and the future appears bleak.
For some, especially those with prior traumatic medical experiences, the DVT diagnosis can ignite symptoms reminiscent of post‑traumatic stress disorder (PTSD). Flashbacks of hospital stays, hyper‑vigilance about physical sensations, and avoidance of medical settings are not uncommon.
Key Psychological Conditions Linked to DVT
Below is a quick snapshot of the most frequently observed mental‑health outcomes after a DVT diagnosis.
| Condition | Core Symptoms | Typical Onset | Impact on Treatment Adherence |
|---|---|---|---|
| Anxiety | Persistent worry, heart‑racing, difficulty sleeping | Hours to days after diagnosis | May lead to missed medication doses |
| Depression | Low mood, loss of interest, fatigue | Weeks after diagnosis | Reduces motivation for follow‑up appointments |
| Health‑Related PTSD | Flashbacks, avoidance of medical care, hyper‑vigilance | Months, especially after a severe complication | Can cause complete disengagement from care |
What Influences the Psychological Impact?
Not every patient reacts the same way. Several factors shape how intense the emotional response becomes.
- Previous Health Experiences: Individuals who have endured prior serious illnesses often have a heightened sense of vulnerability.
- Risk Factor Awareness: Knowing that immobility, recent surgery, or genetic clotting disorders increase DVT risk can either empower patients (through control) or amplify fear.
- Support System Quality: A strong network of family, friends, or online forums buffers stress, while isolation magnifies it.
- Information Delivery: Clear, compassionate communication from clinicians reduces uncertainty. Jargon‑heavy explanations tend to increase anxiety.
- Socio‑Economic Context: Access to medication, ability to take time off work, and insurance coverage affect both physical and mental health outcomes.
Tools and Strategies to Manage the Emotional Fallout
Below are practical steps that patients can adopt right after hearing the diagnosis.
- Ask for a Simple Explanation: Request that the provider describe the clot, its location, and the treatment plan in plain language. Understanding the "why" behind anticoagulant therapy (anticoagulant therapy medications that thin the blood to prevent clot growth and new clots) reduces the unknown.
- Schedule a Mental‑Health Check: Many vascular clinics now embed a brief screening for anxiety or depression during the first visit. If you’re flagged, ask for a referral to a psychologist or psychiatrist.
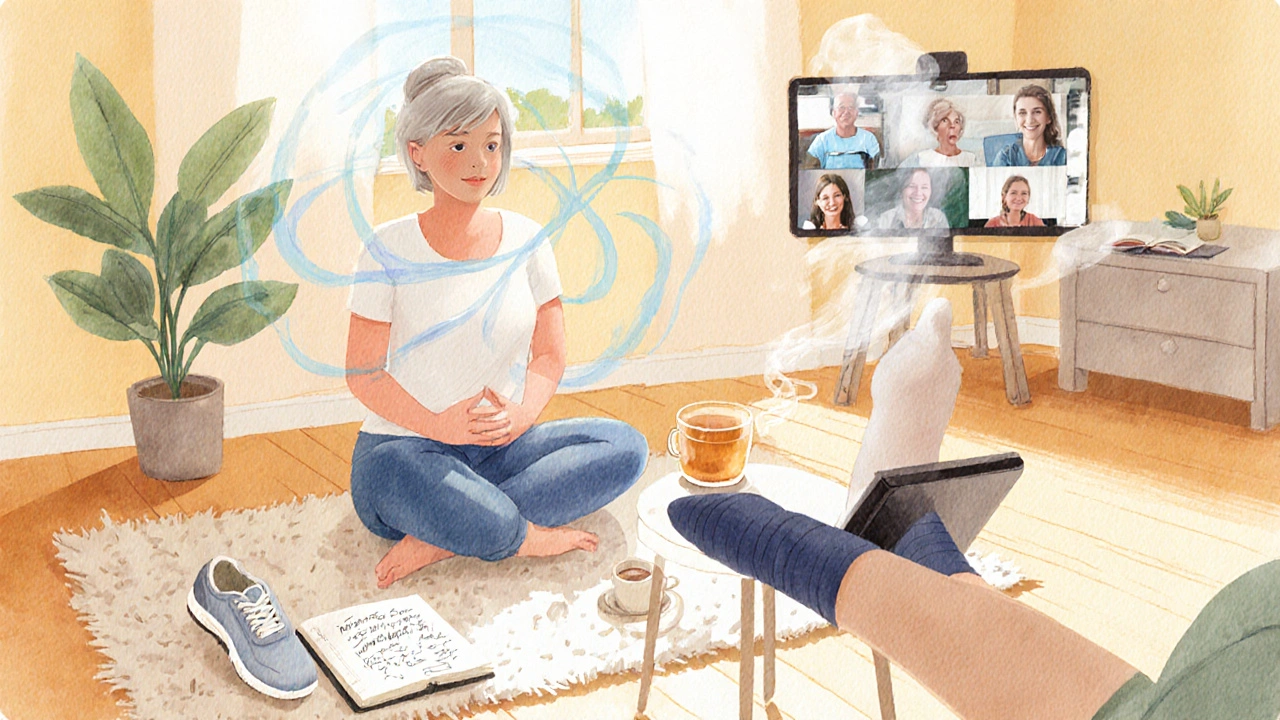
- Use Mind‑Body Techniques: Guided breathing, progressive muscle relaxation, or short mindfulness apps have been shown to lower short‑term anxiety scores in DVT patients.
- Stay Physically Active Within Limits: Light walking, ankle pumps, and prescribed compression stockings improve circulation and boost mood. Consult your physiotherapist for a safe regimen.
- Connect with Others: Join a patient support group online or in‑person community where members share experiences, coping tricks, and encouragement. Hearing stories of successful recovery can replace catastrophic thinking.
- Track Your Thoughts: Journaling about fears-especially health‑related anxiety-helps you identify patterns, challenge irrational beliefs, and gradually reframe them.
- Limit Over‑Research: While information is empowering, endless Googling can fuel health anxiety. Pick reputable sources like the American Heart Association or your physician’s handouts.

The Role of Healthcare Providers
Doctors, nurses, and pharmacists aren’t just there to prescribe a venous ultrasound imaging test that visualizes clots in deep veins or dispense blood thinners. They also act as first‑line mental‑health allies.
Best practices include:
- Delivering the diagnosis in a private, calm setting.
- Using lay terms and checking for understanding.
- Offering written summaries that cover both medical and emotional coping tips.
- Screening for anxiety, depression, and PTSD using brief tools like GAD‑7 or PHQ‑9.
- Referring patients to mental‑health professionals when scores are moderate or higher.
- Scheduling a follow‑up call within a week to address lingering worries.
When clinicians acknowledge the emotional weight of a DVT diagnosis, patients report higher satisfaction and better adherence to anticoagulant regimens.
Resources You Can Turn To Right Now
Here’s a quick checklist of places you can find reliable help.
- National Blood Clot Alliance (NBCA): Offers printable guides, webinars, and a moderated forum for patients.
- American Psychological Association (APA) - Find a Therapist: Search by specialty in health anxiety or chronic illness coping.
- Local Hospital Social Work Departments: Many provide free counseling sessions for recent diagnoses.
- Mobile Apps: “Calm” and “Headspace” have specific modules for medical anxiety.
- Physical Therapy Clinics: Can design safe, clot‑friendly activity plans to keep you moving.
When to Seek Immediate Help
If you notice any of the following, contact your care team or emergency services right away:
- Sudden shortness of breath, chest pain, or coughing up blood-possible pulmonary embolism.
- Severe, unrelenting anxiety that leads to panic attacks and inability to function.
- Thoughts of self‑harm or hopelessness-reach out to a crisis line immediately.
Quick medical attention not only prevents physical complications but also opens the door for urgent mental‑health support.
Frequently Asked Questions
Can a DVT diagnosis cause long‑term depression?
Yes, especially if the clot leads to lifestyle restrictions or recurrent medical scares. Studies show about 20% of DVT patients develop depressive symptoms that persist beyond six months unless they receive counseling or medication.
Is it normal to feel panic after a venous ultrasound?
Feeling a spike of panic is common because the test highlights the clot’s size and location. Knowing the results can actually reduce anxiety, so ask the technician to explain what they see in simple terms.
How soon should I talk to a therapist after diagnosis?
Ideally within the first two weeks. Early intervention helps prevent the escalation of anxiety or depressive thoughts and supports better medication adherence.
Do support groups really help?
Yes. Peer groups provide validation, practical tips, and a sense of community. A 2023 survey of 800 DVT survivors found that participants in support groups reported 30% lower anxiety scores.
Can lifestyle changes reduce the chance of future clots?
Absolutely. Regular low‑impact exercise, maintaining a healthy weight, staying hydrated, and using compression stockings when advised all lower recurrence risk, which in turn eases mental stress.


Post A Comment