Addison's Disease Dose Calculator
This tool helps you calculate appropriate hydrocortisone replacement doses for Addison's disease management. Dosing should always be individualized with your healthcare provider.
Results
Based on standard guidelines for Addison's disease management
When the body’s main stress hormone drops, life can feel like a constant uphill battle. That’s exactly what happens in Addison’s disease, a rare form of adrenal insufficiency where the adrenal glands can’t produce enough cortisol. This guide breaks down why cortisol matters, how its deficiency triggers symptoms, and what you can do to keep the balance right.
Quick Takeaways
- Cortisol is the key glucocorticoid that regulates metabolism, blood pressure, and the stress response.
- Addison’s disease is an autoimmune or infectious destruction of the adrenal glands, leading to low cortisol and often low aldosterone.
- Diagnosis hinges on morning cortisol levels and ACTH stimulation tests.
- Treatment usually involves lifelong hydrocortisone (a synthetic cortisol) and sometimes fludrocortisone for mineralocorticoid support.
- Patients must adjust doses during illness, surgery, or high‑stress events to avoid adrenal crisis.
What Is Cortisol?
Cortisol is a glucocorticoid hormone produced by the adrenal cortex that helps control metabolism, immune response, and the body’s reaction to stress. It follows a diurnal rhythm, peaking in the early morning (around 8am) and dipping to its lowest at night. Cortisol binds to glucocorticoid receptors in almost every cell, influencing glucose production, blood‑vessel tone, and inflammatory pathways.
Key attributes of cortisol:
- Biological half‑life: roughly 60‑90 minutes.
- Potency: considered the reference standard (1×) for glucocorticoid activity.
- Mineralocorticoid effect: modest, helps retain sodium.
Addison’s Disease in a Nutshell
Addison's disease is a chronic condition where the adrenal glands fail to produce sufficient cortisol and, in many cases, aldosterone, leading to adrenal insufficiency. The most common cause in developed countries is autoimmune adrenalitis-your immune system mistakenly attacks the adrenal cortex. Infections (like tuberculosis) and rare genetic mutations are other culprits.
Typical signs include chronic fatigue, muscle weakness, weight loss, low blood pressure, salt cravings, and hyperpigmentation of the skin. Because cortisol supports blood‑sugar regulation, patients may experience frequent hypoglycemia, especially after skipping meals.
How Cortisol Links to Addison’s Disease
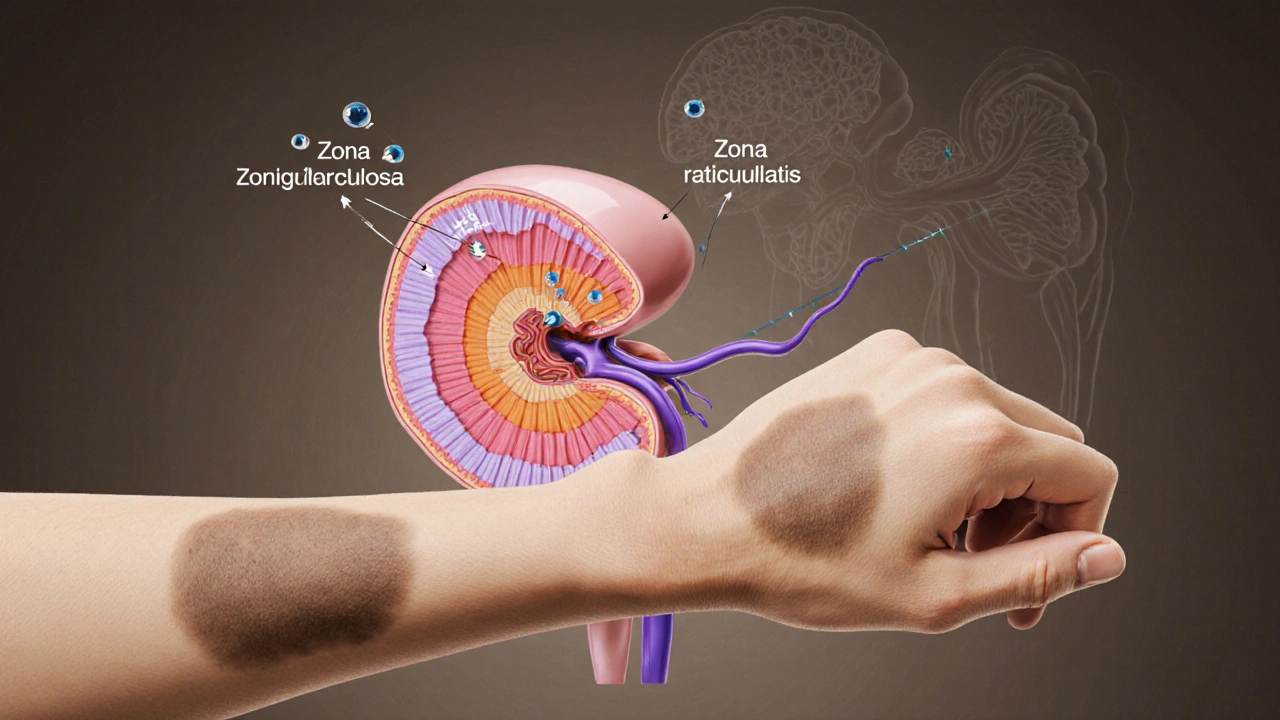
The adrenal cortex sits atop the kidneys and consists of three zones: zona glomerulosa (produces aldosterone), zona fasciculata (produces cortisol), and zona reticularis (produces androgens). In Addison’s disease, the adrenal gland is the small, triangular organ responsible for making cortisol, aldosterone, and adrenal androgens is damaged, so the zona fasciculata can’t make enough cortisol.
The hypothalamic‑pituitary‑adrenal (HPA axis is the feedback loop linking the brain, pituitary gland, and adrenal cortex to regulate cortisol production) tries to compensate. The hypothalamus releases corticotropin‑releasing hormone (CRH), prompting the pituitary to secrete adrenocorticotropic hormone (ACTH). In primary adrenal failure, ACTH levels sky‑rocket because the adrenal gland doesn’t respond, which explains the characteristic darkening of the skin-ACTH stimulates melanocytes.
Low cortisol means:
- Reduced gluconeogenesis → low blood sugar.
- Weaker vascular tone → orthostatic hypotension.
- Impaired anti‑inflammatory control → exaggerated immune reactions.
- Decreased sodium reabsorption (if aldosterone is also low) → dehydration and electrolyte imbalance.
Diagnosing Cortisol Deficiency
Doctors rely on a combination of clinical clues and lab tests. The first step is a morning serum cortisol measured before 9am.
- Low cortisol (<8µg/dL) strongly suggests adrenal insufficiency.
- Intermediate values (8‑18µg/dL) often trigger an ACTH stimulation test.
The ACTH stimulation test involves administering synthetic ACTH (cosyntropin) and measuring cortisol response at 30 and 60 minutes is the gold standard. A rise to >18‑20µg/dL usually rules out primary Addison’s; a blunted response confirms it.
Other useful measurements:
- Plasma ACTH - high in primary failure, low/normal in secondary. \n
- Renin and aldosterone - elevated renin with low aldosterone points to combined glucocorticoid‑mineralocorticoid loss.
Treatment: Replacing the Missing Hormone
The cornerstone of therapy is oral hydrocortisone a synthetic form of cortisol used to mimic the natural hormone’s daily rhythm. Typical dosing mimics the body’s diurnal curve: a larger dose in the morning (10‑20mg) and a smaller one in the afternoon (5‑10mg). Split dosing reduces the risk of fatigue and helps maintain blood pressure.
When aldosterone is also deficient, physicians add fludrocortisone a synthetic mineralocorticoid that restores sodium balance and blood pressure, usually 0.05‑0.1mg daily.
Monitoring involves checking morning cortisol, electrolytes, and blood pressure every few months. Patients also keep a stress‑dose kit (usually 100mg hydrocortisone tablets) to inject intramuscularly during severe illness or injury.

Comparing Natural Cortisol with Common Synthetic Glucocorticoids
| Drug | Relative potency | Half‑life (hours) | Mineralocorticoid activity | Typical daily dose (adult) |
|---|---|---|---|---|
| Hydrocortisone (cortisol) | 1× | 0.8‑1.5 | Moderate | 15‑30mg |
| Prednisolone | 4‑5× | 2‑3 | Low | 5‑10mg |
| Dexamethasone | 25‑30× | 36‑54 | None | 0.5‑1mg |
Hydrocortisone remains the drug of choice for Addison’s because its activity and half‑life best mimic natural cortisol, reducing the risk of overtreatment and bone loss.
Living with Addison’s: Stress Management and Lifestyle Tips
Since cortisol is the main stress‑hormone, patients must plan for any situation that spikes demand:
- Illness: Double the morning hydrocortisone dose and keep the injection kit handy.
- Surgery or dental work: Administer 100mg hydrocortisone IV before the procedure, then resume oral dosing after recovery.
- Extreme exercise or heat exposure: Add a 5‑10mg boost if you feel dizzy or nauseated.
Nutrition also plays a role. A salt‑rich diet helps when aldosterone is low, while balanced meals prevent hypoglycemia. Regular moderate exercise improves cardiovascular tone without triggering an adrenal crisis.
Common Pitfalls and How to Avoid Them
Even with proper medication, mistakes happen:
- Skipping doses: Missing a morning tablet can cause rapid fatigue; set phone reminders.
- Using the wrong stress‑dose form: Only hydrocortisone tablets are approved for emergency injection; glucocorticoids like prednisolone are not interchangeable.
- Over‑supplementing: Chronic high doses increase infection risk and bone loss; keep dose adjustments short‑term.
- Ignoring electrolyte signs: Muscle cramps or low blood pressure may mean aldosterone deficiency-check sodium intake and consider fludrocortisone adjustment.
Regular follow‑ups with an endocrinologist ensure lab values stay within target and that your stress‑dose kit is up‑to‑date.
Frequently Asked Questions
Why does my skin get darker with Addison’s disease?
The failing adrenal glands can’t make cortisol, so the pituitary releases excess ACTH. ACTH shares a precursor (POMC) with melanocyte‑stimulating hormone (MSH), which triggers melanin production and darkens the skin, especially in sun‑exposed areas.
Can I take prednisone instead of hydrocortisone?
Prednisone is much more potent and has a longer half‑life, so it can over‑suppress the immune system and cause bone loss. For primary adrenal insufficiency, hydrocortisone (or cortisone acetate) is preferred because it mimics natural cortisol’s timing and strength.
Do I need to wear a medical alert bracelet?
Yes. An alert bracelet or necklace quickly informs emergency responders that you have adrenal insufficiency, prompting them to give IV hydrocortisone if you can’t communicate.
How often should I get my cortisol levels checked?
After the initial diagnosis, most endocrinologists review cortisol, ACTH, electrolytes, and blood pressure every 6‑12 months, unless you change doses or develop new symptoms.
What is the difference between primary and secondary adrenal insufficiency?
Primary (Addison’s) means the adrenal glands themselves are damaged, causing low cortisol **and** low aldosterone, with high ACTH. Secondary insufficiency comes from pituitary or hypothalamic problems; cortisol is low but aldosterone often stays normal because the renin‑angiotensin system remains intact, and ACTH is low or normal.
Understanding how cortisol works-and why its absence wreaks havoc-empowers you to take charge of Addison’s disease. With the right testing, medication, and emergency plan, you can keep the hormone balance in check and live a full, active life.


Post A Comment