Mood Disorders: Understanding, Managing, and Finding Help
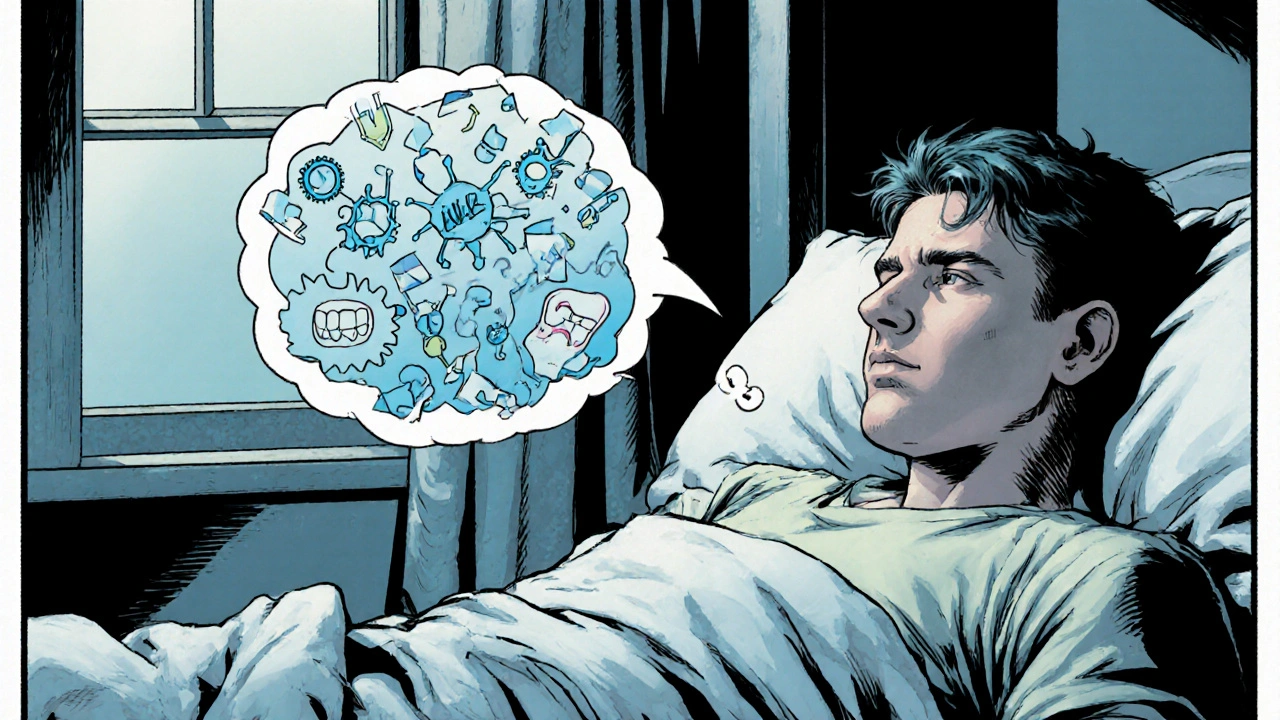
When dealing with Mood Disorders, a group of conditions that cause persistent emotional highs or lows. Also known as affective disorders, they affect how you feel, think, and handle daily activities. This umbrella term covers a range of experiences, from the heavy cloud of Depression, a common mood disorder marked by prolonged sadness and loss of interest to the roller‑coaster swings of Bipolar Disorder, a condition that alternates between depressive lows and manic highs. To tackle these challenges, many turn to Antidepressants, medications that balance brain chemicals and lift mood or to Antipsychotics, drugs that help stabilize extreme mood swings and psychotic symptoms. Understanding how these pieces fit together is the first step toward regaining control.
mood disorders don’t just happen in a vacuum; they intersect with lifestyle, genetics, and stress. A family history of depression can double your risk, while chronic sleep loss or an anxiety disorder often fuels mood swings. The brain’s serotonin, dopamine, and norepinephrine pathways act like a thermostat for emotions—when they’re out of sync, you feel the impact. For many, a simple blood test won’t reveal the issue, but a thorough clinical interview can uncover patterns that guide treatment. That’s why professionals use tools like the PHQ‑9 questionnaire to gauge severity and track progress over time.
Key Factors that Influence Mood Disorders
First, genetics set the stage. Studies show that if a first‑degree relative has bipolar disorder, you’re up to ten times more likely to develop it yourself. Second, environmental triggers—such as traumatic events, relationship breakdowns, or job loss—can spark an episode even in someone without a strong genetic load. Third, physical health plays a big role; thyroid imbalances, vitamin D deficiency, and chronic illnesses like diabetes often aggravate mood symptoms. Finally, lifestyle habits—exercise, diet, and social connection—can either buffer or exacerbate the condition. Small tweaks, like a daily walk or a balanced omega‑3 intake, have been shown to improve treatment response.
Medication isn’t a one‑size‑fits‑all solution. Selective serotonin reuptake inhibitors (SSRIs) like fluoxetine are first‑line for many with depression, while lithium remains the gold standard for stabilizing bipolar mania. Newer agents, such as atypical antipsychotics (e.g., olanzapine or quetiapine), serve dual purposes: they calm manic episodes and sometimes help with depressive phases. It’s crucial to match the drug’s mechanism to the specific symptom profile—this is where a psychiatrist’s expertise shines. Side‑effects vary: weight gain, sleepiness, or sexual dysfunction can deter adherence, so open communication about concerns is essential.
Beyond pills, psychotherapy offers a powerful complement. Cognitive‑behavioral therapy (CBT) teaches you to spot distorted thoughts and replace them with realistic alternatives. For bipolar disorder, interpersonal‑and‑social‑rhythm therapy (IPSRT) focuses on stabilizing daily routines to prevent mood swings. Many patients benefit from a blended approach—medication to address biology and therapy to reshape thinking patterns. Support groups also provide a sense of community, reducing the isolation that often accompanies mood disorders.
When you’re navigating a new diagnosis, practical steps can make a huge difference. Keep a mood journal to log triggers, sleep, diet, and medication timing; patterns that emerge can guide your clinician’s adjustments. Build a crisis plan: identify warning signs, trusted contacts, and emergency services. Don’t overlook the importance of regular medical check‑ups—some medications require liver function monitoring or blood level checks. And remember, recovery isn’t linear; setbacks happen, but they don’t erase progress.
Our collection of articles below dives deeper into each of these topics. You’ll find a detailed comparison of antipsychotic options like Olanzapine, guidance on how antidepressants such as Celexa work, coping strategies for the emotional toll of chronic illnesses, and practical tips for managing mood symptoms in everyday life. Whether you’re looking for medication reviews, lifestyle hacks, or mental‑health support resources, the posts ahead offer clear, actionable information.
Ready to explore more? Scroll down to discover expert‑backed guides that break down treatment choices, reveal hidden side‑effects, and share real‑world coping tactics—everything you need to take control of your mental well‑being.
How Enzyme Deficiencies Trigger Depression and Anxiety
Explore how enzyme deficiencies can cause depression and anxiety, learn key enzymes, gut links, nutrient support, and actionable steps to improve mood.
Read More