Mood Enzyme Support Calculator
Vitamin B6
Supports GAD enzyme activity and serotonin synthesis
Magnesium
Supports serotonin & dopamine synthesis pathways
Zinc
Supports MAO-A & COMT enzyme function
Imagine waking up feeling low, anxious, and unable to focus, and the cause isn’t a chemical imbalance in your brain but a missing piece in the body’s biochemical toolkit. That missing piece is often an enzyme deficiency. When key enzymes don’t do their job, the cascade of neurotransmitters, hormones, and immune signals can go off‑track, leading straight into the territory of depression and anxiety.
What enzymes are and why they matter
When we talk about Enzyme - a biological catalyst that speeds up chemical reactions in the body, we’re dealing with the tiny machines that keep every cell running. Without enzymes, even simple processes like breaking down food or synthesizing neurotransmitters would take forever, and many reactions would never happen at all.
Understanding enzyme deficiency
Enzyme deficiency - a condition where the body lacks enough functional enzyme to carry out a specific biochemical reaction efficiently can arise from genetics, poor nutrition, chronic stress, or gut imbalances. The result? A bottleneck in the pathways that create mood‑regulating chemicals.
Neurotransmitters that rely on enzymes
Three brain chemicals dominate mood regulation: serotonin, dopamine, and GABA. Each one needs a dedicated enzyme to be made or broken down.
- Serotonin - a neurotransmitter that promotes feelings of well‑being and happiness is synthesized from the amino acid tryptophan by the enzyme tryptophan hydroxylase (TPH). If TPH activity drops, serotonin levels fall, paving the way for low mood.
- Dopamine - the brain’s reward chemical that drives motivation and pleasure is produced in a two‑step process involving tyrosine hydroxylase (TH) and aromatic L‑amino acid decarboxylase (AADC). Deficiencies in TH can blunt motivation and spark anhedonia.
- GABA - the main inhibitory neurotransmitter that calms neuronal firing is generated from glutamate by glutamic acid decarboxylase (GAD). Low GAD activity is frequently linked to heightened anxiety.
Key enzymes most often linked to mood disorders
| Enzyme | Primary Function | What Happens When Low? | Typical Mood Impact |
|---|---|---|---|
| MAO‑A (Monoamine Oxidase A) | Breaks down serotonin, dopamine, norepinephrine | Build‑up of monoamines or, paradoxically, depletion if co‑factors missing | Can cause anxiety spikes or depressive crashes |
| COMT (Catechol‑O‑methyltransferase) | Metabolises dopamine and norepinephrine | Reduced clearance leads to erratic dopamine signaling | Impaired concentration, mood swings |
| GAD (Glutamic Acid Decarboxylase) | Converts glutamate to GABA | Less GABA, more excitatory activity | Heightened anxiety, irritability |
| TPH2 (Tryptophan Hydroxylase 2) | First step in brain serotonin synthesis | Reduced serotonin production | Depressive symptoms, low appetite |
These four enzymes form a core map that many clinicians use when investigating treatment‑resistant mood disorders. If a patient’s labs show low activity of any of these, supplementing cofactors (like vitamin B6 for GAD) or prescribing enzyme‑targeted medications can shift the balance dramatically.
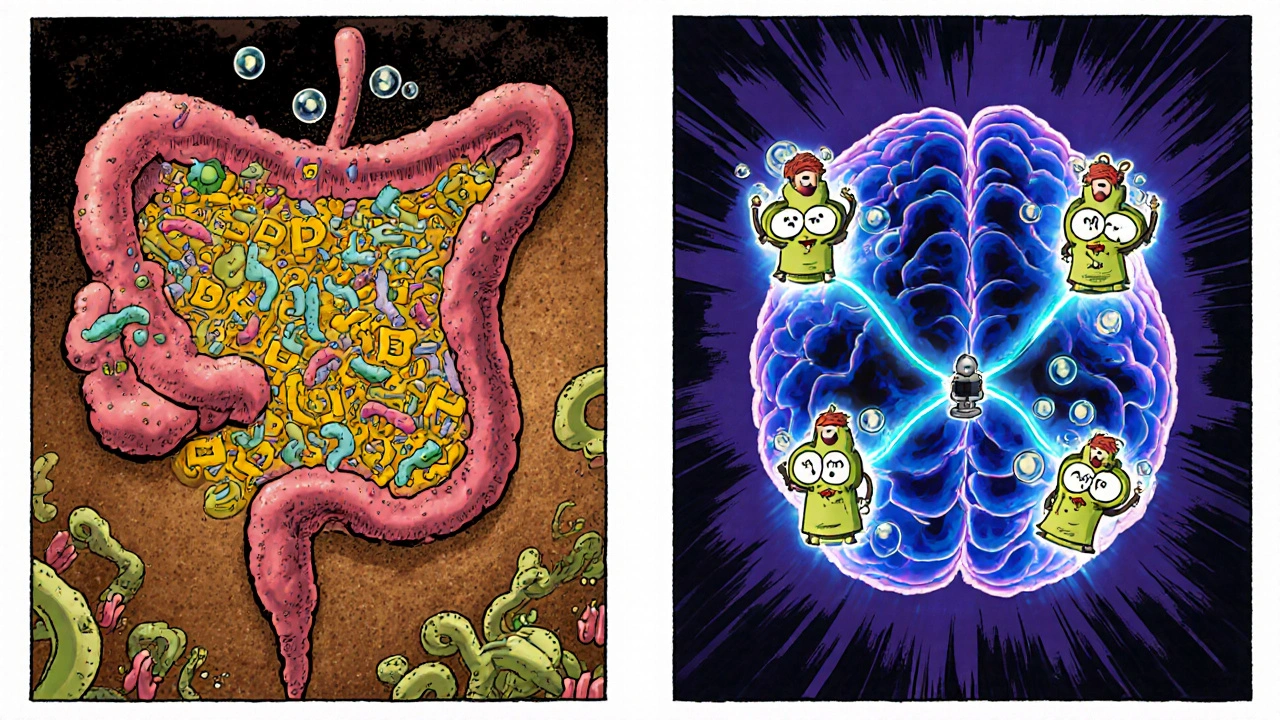
The gut microbiome’s role in enzyme availability
Your gut is more than a digestion chamber; it’s an enzyme factory. The Gut microbiome - the community of trillions of bacteria living in the digestive tract that help break down food and produce nutrients produces vitamins (B‑complex, K) and short‑chain fatty acids that act as cofactors for the brain‑related enzymes above. Dysbiosis-an imbalance in gut bacteria-can lower the production of these cofactors, indirectly starving enzymes like GAD and TPH2.
Studies from 2023‑2024 show that people with chronic anxiety often have reduced levels of Lactobacillus and Bifidobacterium, both of which aid in synthesizing B vitamins needed for neurotransmitter enzymes. Restoring a healthy microbiome with probiotic‑rich foods or targeted supplements can lift enzyme activity and calm the nervous system.
Nutrients that fuel enzyme function
Even with a balanced gut, you still need the right building blocks. Here are the top three nutrients that act as enzyme cofactors for mood regulation:
- Vitamin B6 - helps convert amino acids into neurotransmitters and is essential for GAD activity. Food sources: chickpeas, salmon, bananas.
- Magnesium - supports over 300 enzymatic reactions, including those that regulate serotonin and dopamine synthesis. Food sources: pumpkin seeds, dark leafy greens, almonds.
- Zinc - crucial for the activity of MAO‑A and COMT enzymes. Food sources: oysters, beef, lentils.
Testing blood levels of these nutrients can pinpoint whether a deficiency is likely contributing to mood symptoms.
Everyday habits that protect enzyme health
- Eat a varied, whole‑food diet. Processed foods often lack the micronutrients enzymes need.
- Manage stress. Chronic cortisol spikes can suppress the production of enzymes like TPH2.
- Prioritise sleep. During deep sleep, the liver ramps up detox enzymes that keep neurotransmitter balance stable.
- Stay hydrated. Water is the medium for all enzymatic reactions; dehydration can slow them down.
- Limit alcohol. Excess alcohol impairs liver enzymes responsible for processing mood‑related hormones.
Small tweaks add up. Most people notice a measurable lift in mood after just two weeks of consistent changes.

When to seek professional help
If you’ve tried diet tweaks, sleep hygiene, and stress‑reduction techniques for more than a month and still feel stuck, it’s time to bring a clinician into the picture. Look for providers who can order:
- Comprehensive metabolic panels that include B‑vitamin and mineral levels.
- Genetic tests for enzyme polymorphisms (e.g., COMT Val158Met).
- Gut microbiome analysis to spot dysbiosis.
Bottom line
Missing or under‑performing enzymes can tip the scales toward depression and anxiety just as much as a stressful job or a traumatic event. By checking nutrient status, supporting gut health, and keeping lifestyle stress low, you give your enzymes the chance to do what they’re built for-keep your mood stable and your mind clear.
Frequently Asked Questions
Can a simple blood test reveal enzyme deficiencies linked to depression?
Standard panels can measure vitamins and minerals that serve as cofactors, but they don’t directly measure enzyme activity. Specialized labs can assess specific enzymes like MAO‑A or COMT through functional assays or genetic testing.
Are probiotic supplements effective for fixing enzyme‑related mood issues?
They can help if your gut flora is the root cause. Strains such as Lactobacillus rhamnosus and Bifidobacterium longum have shown promise in boosting B‑vitamin production, which in turn supports neurotransmitter enzymes.
What lifestyle change gives the biggest boost to enzyme function?
Regular, balanced meals rich in B‑vitamins and magnesium combined with adequate sleep (7‑9hours) provides the most consistent enzyme support. Stress reduction is a close second.
Is it safe to self‑prescribe enzyme‑boosting supplements?
Most nutrients are safe at recommended doses, but high levels of magnesium or zinc can interfere with medication absorption. Always check with a healthcare professional before starting a new regimen.
Can genetics lock me out of having normal enzyme levels?
Certain gene variants (e.g., COMT Val/Met) reduce enzyme efficiency, but diet, lifestyle, and targeted supplements can often compensate for the shortfall.

Post A Comment