Calcium and Its Role in Health
When working with calcium, a vital mineral that builds and maintains strong bones and teeth. Also known as Ca, it supports muscle function, nerve signaling, and blood clotting. Most people think of dairy as the main source, but leafy greens, fortified foods, and supplements all count. Understanding how calcium fits into the bigger picture helps you make smarter choices, whether you’re preventing a break, managing a condition, or just staying active.
How Vitamin D Powers Calcium Absorption
Enter vitamin D, a fat‑soluble vitamin that enhances calcium uptake in the gut. Without enough vitamin D, even a diet rich in calcium can leave you deficient. Sunlight, fatty fish, and fortified products are the easiest ways to raise levels, but many adults need a supplement during winter months. The synergy between calcium and vitamin D is a classic example of a nutrient pair where one unlocks the other's benefit.
The next big connection is with osteoporosis, a condition marked by porous, fragile bones due to low calcium density. Studies show that maintaining adequate calcium intake, especially when paired with vitamin D, can slow bone loss and reduce fracture risk. For post‑menopausal women and older men, this duo becomes a daily defense line. Lifestyle factors like weight‑bearing exercise and limiting excess sodium also tip the scale toward stronger bones.
Beyond bone health, calcium interacts with many common supplements and medications. For instance, high‑dose iron or zinc can compete for absorption, lowering the amount your body actually uses. Certain diuretics increase calcium loss through urine, while some thyroid medications affect calcium metabolism. Knowing these supplement interactions lets you space doses or choose formulations that minimize conflict.
Practical tips start with checking your current intake. A quick food diary for a week often reveals gaps—maybe you skip dairy or rely heavily on processed foods. If you’re under 50 and eat a balanced diet, you might meet the Recommended Dietary Allowance (RDA) of 1,000 mg per day. Above that age, aim for 1,200 mg, and consider a calcium citrate supplement if you have low stomach acid. Remember, more isn’t always better; excess calcium can raise kidney stone risk, so balance is key.
Finally, keep an eye on laboratory results. Serum calcium, parathyroid hormone (PTH), and vitamin D levels together paint a clear picture of how well your body is handling the mineral. If any numbers look off, a healthcare provider can adjust diet, supplements, or medications accordingly. With the right mix of food, sunshine, and smart supplementation, you’ll give your bones the support they need and lower the chance of osteoporosis down the line.
Below you’ll find a curated list of articles that dig deeper into genetics, drug comparisons, diet strategies, and more—all connected to the calcium theme. Browse the collection to see how this mineral ties into everything from mental health to infection risk, and pick the pieces that match your health goals.
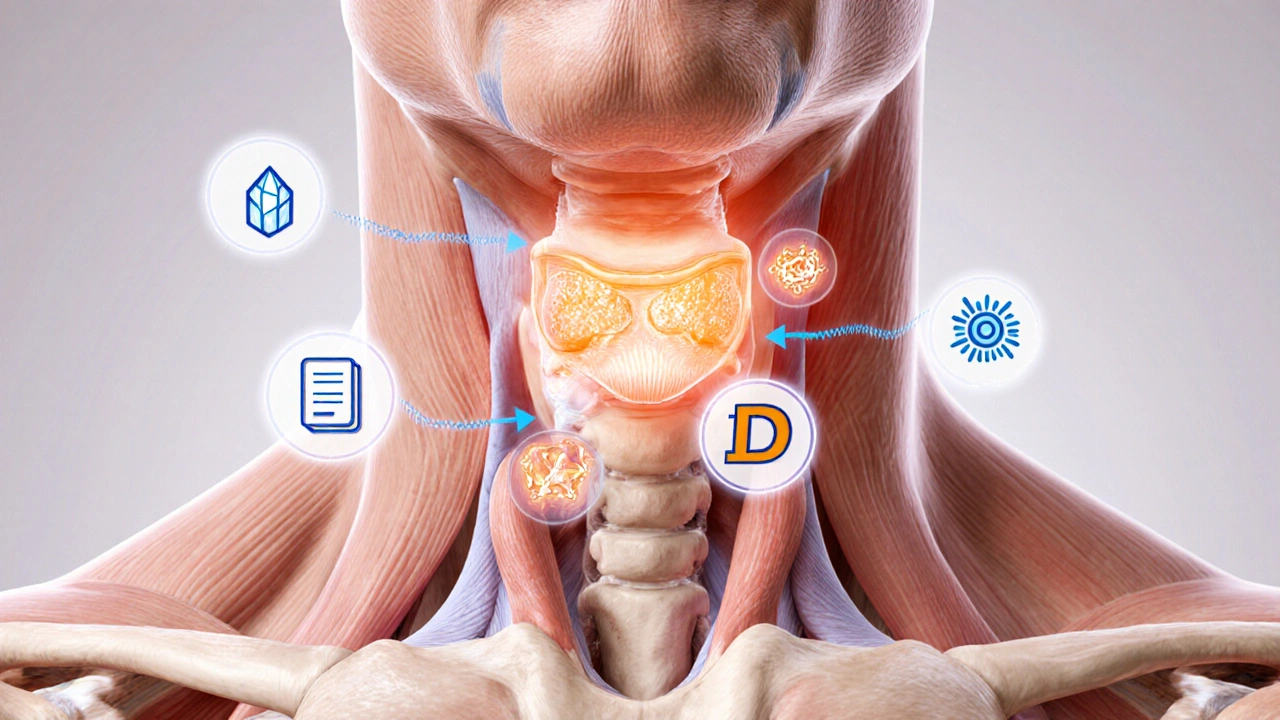
Calcium, Vitamin D & Secondary Hyperparathyroidism: What You Need to Know
Learn how calcium and vitamin D work together to manage secondary hyperparathyroidism, with diet tips, supplement guidelines, lab monitoring and FAQs.
Read More