Antipsychotics: What They Are, How They Work, and What You Need to Know
When someone is struggling with hallucinations, delusions, or severe mood swings, antipsychotics, a class of medications designed to reduce symptoms of psychosis by balancing brain chemicals like dopamine. Also known as neuroleptics, these drugs don’t cure mental illness—but they can make daily life possible again. Whether it’s for schizophrenia, bipolar disorder, or even severe anxiety with psychotic features, antipsychotics are often the first line of defense when thoughts start to feel out of control.
There are two main types: first-generation and second-generation antipsychotics. First-generation ones, like haloperidol, work mainly by blocking dopamine, but they often cause movement problems like tremors or stiffness. Second-generation drugs, like risperidone or olanzapine, target both dopamine and serotonin, which usually means fewer movement side effects—but they can lead to weight gain, high blood sugar, or high cholesterol. The choice isn’t about which is "better," but which fits the person’s body, lifestyle, and symptoms. Some people need to try a few before finding the right one, and that’s normal.
Antipsychotics don’t work like painkillers—you won’t feel better right away. It often takes weeks for symptoms to improve, and even then, the goal isn’t to feel "normal," but to feel stable enough to get back to work, relationships, or just sleeping through the night. Many people stop taking them too soon because they feel fine, not realizing that stopping suddenly can trigger a relapse. That’s why ongoing support from a doctor matters. And if you’re on other meds—like antidepressants, blood pressure pills, or even herbal supplements—those can interact with antipsychotics in dangerous ways. For example, mixing them with alcohol or certain pain meds can raise the risk of heart rhythm problems or extreme drowsiness.
Side effects are real, but they’re not inevitable. Muscle stiffness? Maybe a dose tweak helps. Weight gain? Diet and movement can offset it. Some people find that switching from one antipsychotic to another reduces the worst effects. And if you’re worried about long-term use, there are monitoring tools—like regular blood tests and heart checks—that doctors use to catch problems early. This isn’t about blindly taking pills. It’s about finding the right balance between managing symptoms and protecting your body.
Below, you’ll find real-world stories and practical advice from people who’ve been there: how to handle missed doses, what to do when side effects hit, how to talk to your doctor about switching meds, and why some people react differently to generics. These aren’t theory pieces—they’re lived experiences, backed by medical facts, designed to help you make smarter choices without feeling overwhelmed.
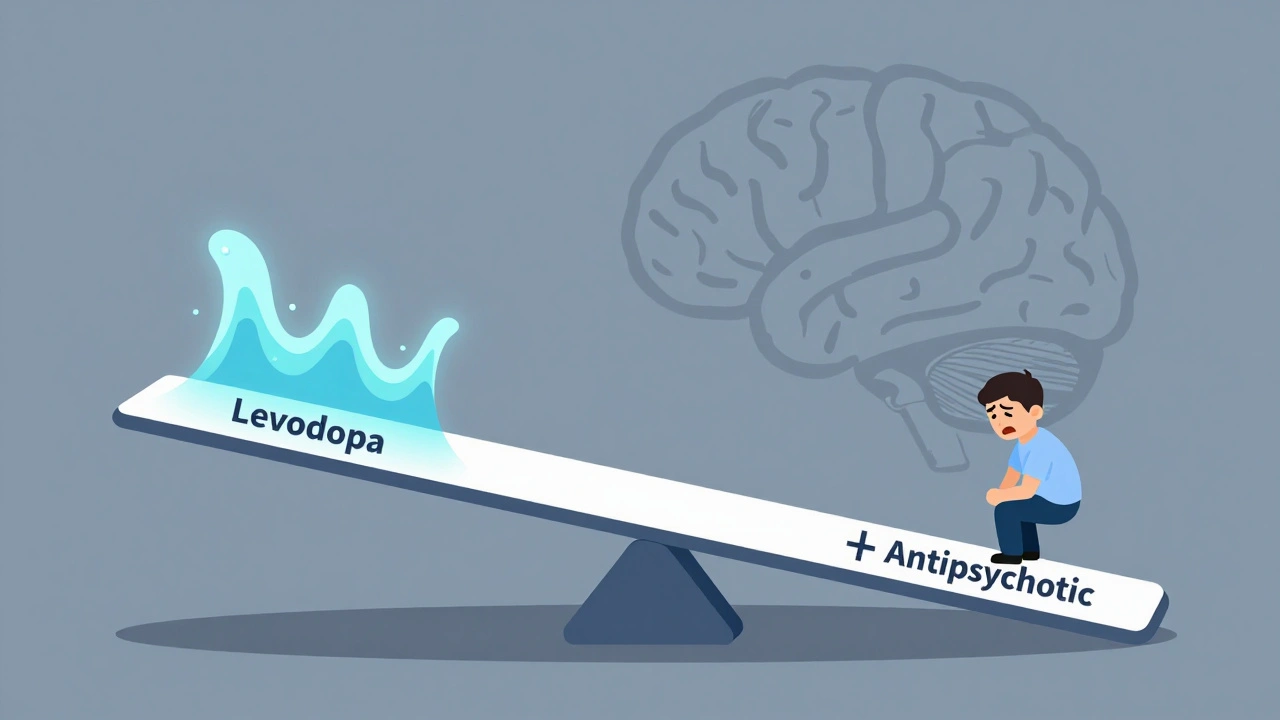
Levodopa and Antipsychotics: How Opposing Dopamine Effects Worsen Symptoms
Levodopa and antipsychotics have opposing effects on dopamine, making it dangerous to use them together. This article explains how this interaction worsens symptoms in Parkinson’s and schizophrenia, and what newer treatments are doing to solve it.
Read More