Lenalidomide Fertility: What You Need to Know
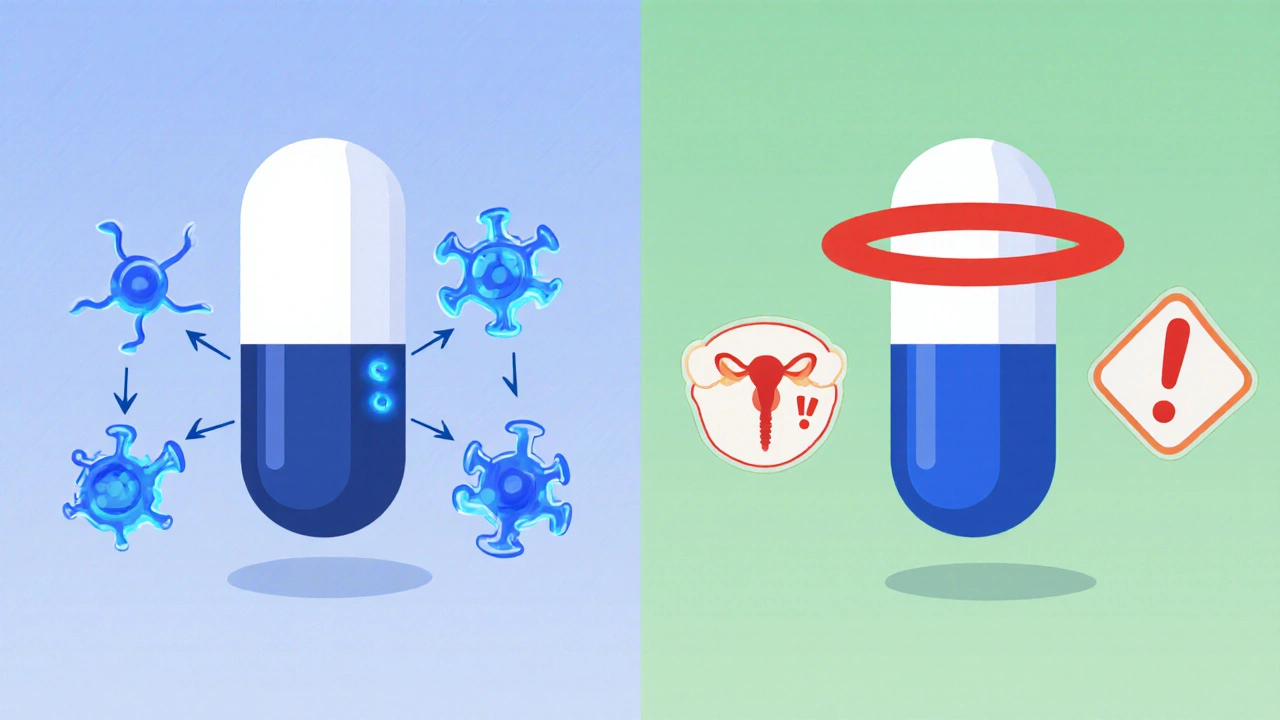
When dealing with lenalidomide fertility, the effect of lenalidomide on a person’s ability to conceive. Also known as lenalidomide reproductive concerns, it raises questions for anyone on a long‑term cancer plan. Lenalidomide, an immunomodulatory drug prescribed for multiple myeloma and certain lymphomas works by altering immune signaling and blood vessel growth. Because it shares a chemical backbone with thalidomide, doctors worry about birth defects, lowered sperm counts, and disrupted ovarian cycles. Fertility, the capacity to reproduce naturally or with assistance can be hit hard by any drug that interferes with hormones or DNA. In patients with multiple myeloma, a cancer of plasma cells that often requires lenalidomide therapy, the treatment goal clashes with the desire to start or grow a family. Adding pregnancy, the state of carrying a developing embryo or fetus into the mix creates a three‑way tug‑of‑war: control the disease, protect future kids, and keep reproductive health intact.
The first step is understanding the drug’s risk profile. Clinical data show that men on lenalidomide may experience a drop in sperm concentration and motility, though some recover after stopping the medication for a few months. Women face a higher teratogenic risk, meaning the drug can cause serious birth defects if exposure happens during the first trimester. Because of this, most guidelines demand a strict birth‑control plan—two reliable methods for at least one month before starting, throughout treatment, and for at least three months after the last dose. Fertility preservation options, such as sperm banking for men or egg freezing for women, become crucial when the treatment timeline is uncertain. Talk with a reproductive specialist early; the sooner you freeze gametes, the better the odds of a healthy future pregnancy.
Beyond the medical checklist, counseling matters. Patients often wonder whether they should pause therapy to try for a baby. The answer isn’t one‑size‑fits‑all. In aggressive disease, pausing could compromise survival, while in remission, a short drug holiday might be safe under close monitoring. The decision hinges on three things: disease status, the patient’s age and reproductive goals, and the availability of preservation methods. For men, semen analysis before, during, and after treatment helps track recovery. For women, hormone‑level testing and ultrasound monitoring guide timing for egg retrieval. If pregnancy does occur while on lenalidomide, the risk of congenital anomalies spikes dramatically, so immediate drug discontinuation and specialist obstetric care are mandatory. In every scenario, a multidisciplinary team—oncologists, fertility doctors, and pharmacists—should weigh the benefits against the risks.
What You’ll Find Below
Below you’ll discover articles that break down the science, share real‑world patient stories, compare preservation techniques, and list the latest guidelines for managing lenalidomide fertility concerns. Whether you’re a patient, a caregiver, or a healthcare professional, the collection gives you practical steps to protect reproductive health while tackling multiple myeloma.
Lenalidomide and Fertility: Risks, Pregnancy Guidelines & What Patients Need to Know
Learn how lenalidomide impacts male and female fertility, the pregnancy risks, and the strict contraception guidelines to follow for safe treatment.
Read More