IMiD Teratogenicity: What You Need to Know
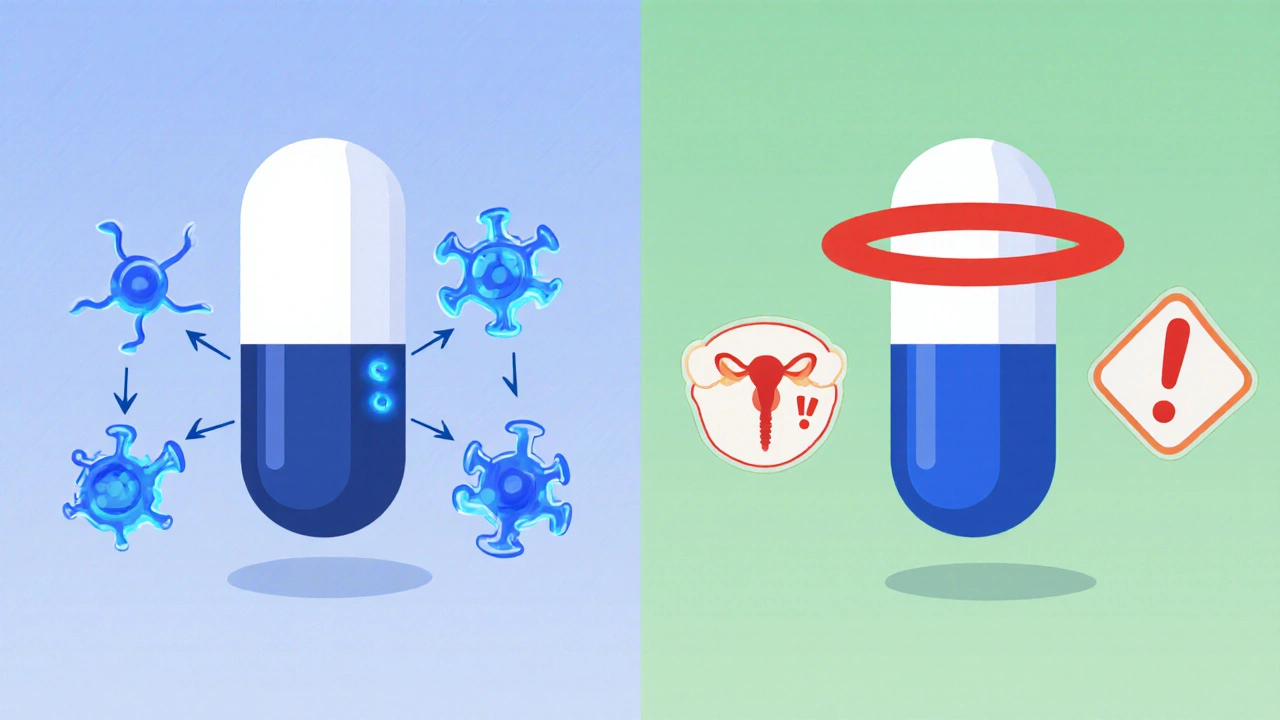
When dealing with IMiD teratogenicity, the risk that immunomodulatory drugs cause birth defects if taken during pregnancy, it’s easy to feel overwhelmed. The term covers a family of medicines – most famously thalidomide, the drug that sparked the modern teratology field after the 1960s tragedy, as well as newer analogs like lenalidomide, used for multiple myeloma and certain blood disorders and pomalidomide, another derivative approved for relapsed disease. All three share a core mechanism that tweaks the immune system, yet each carries a label in the highest pregnancy‑risk category. Because the danger is so clear, doctors and regulators treat IMiD teratogenicity as a non‑negotiable safety checkpoint: patients must enroll in risk‑evaluation programs, undergo regular pregnancy testing, and adhere to strict birth‑control requirements. In practice, this means the drug’s benefits are balanced against a clear, documented danger to a developing fetus, and every prescription triggers a chain of safeguards designed to keep pregnancies out of the exposure window.
The safety net starts with the FDA REMS program, a structured system that mandates education, monitoring, and controlled distribution for high‑risk drugs. Under REMS, pharmacies, prescribers, and patients all sign off on a set of commitments: confirm a negative pregnancy test before each fill, use two forms of contraception, and report any pregnancy that occurs despite precautions. This framework directly addresses the core predicate that "IMiD teratogenicity requires strict pregnancy testing" and creates a feedback loop where adverse events are quickly captured and acted upon. In parallel, the drugs carry the designation of Pregnancy Category X – a legal tag that signals absolute contraindication in pregnancy. The combination of REMS oversight and Category X labeling forms a dual‑layered barrier, ensuring that the risk of birth defects isn’t left to chance. Clinicians also rely on clinical guidelines that outline counseling points: discuss the teratogenic potential openly, document consent, and schedule monthly labs to catch any lapses early. When a patient plans to conceive, the standard protocol is a supervised drug washout period, often spanning weeks, to let the medication clear from the body before trying for a baby.
Beyond paperwork, real‑world care focuses on practical steps that patients can take every day. Using both hormonal and barrier methods simultaneously, keeping a medication diary, and setting calendar reminders for pregnancy tests are simple habits that dramatically lower exposure odds. For women of child‑bearing potential, many specialists recommend enrolling in a pregnancy‑prevention registry, which not only tracks compliance but also contributes data for ongoing safety research. If a pregnancy does slip through, the medical team must act fast: halt the IMiD immediately, involve a teratology information service, and consider fetal monitoring as advised by specialists. All of these measures illustrate how "IMiD teratogenicity influences clinical decision‑making" and why staying informed is crucial for anyone prescribed these agents. Below you’ll find a curated set of articles that dig deeper into specific drugs, regulatory updates, and patient‑focused strategies, giving you a clear roadmap to manage these powerful medicines safely.
Lenalidomide and Fertility: Risks, Pregnancy Guidelines & What Patients Need to Know
Learn how lenalidomide impacts male and female fertility, the pregnancy risks, and the strict contraception guidelines to follow for safe treatment.
Read More