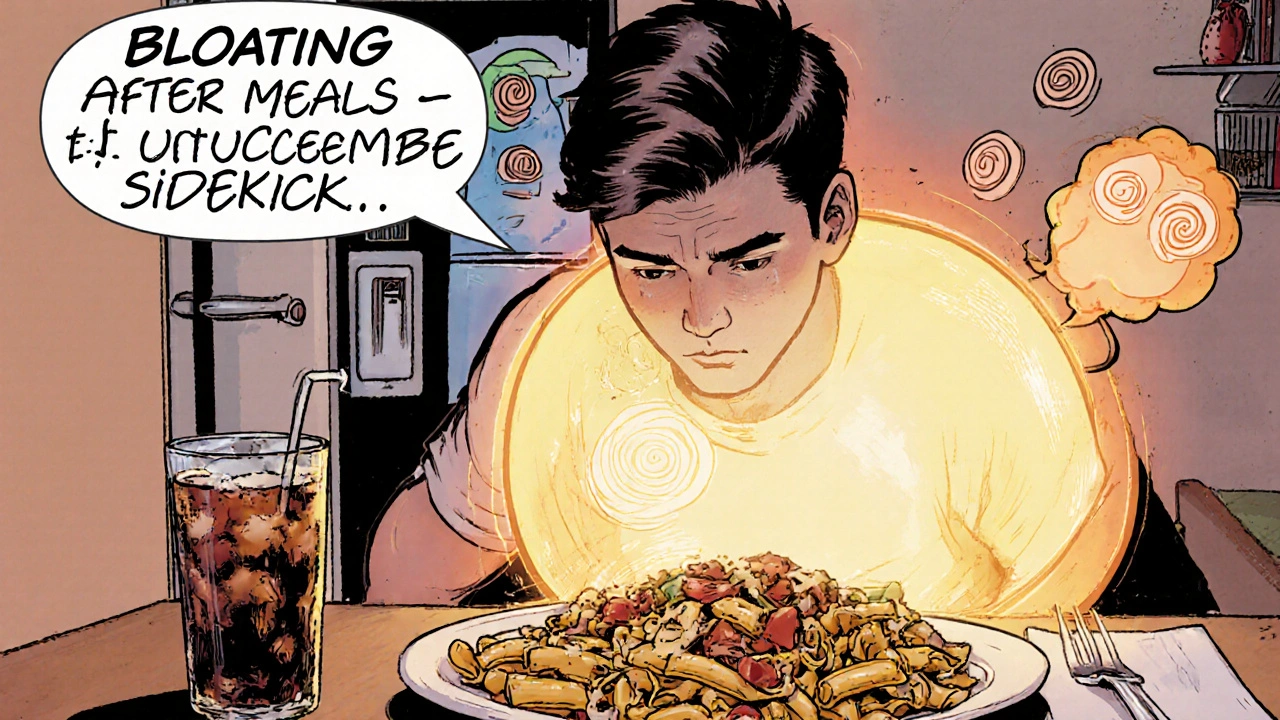
Bloating After Eating – What’s Behind the Fullness?
When dealing with bloating after eating, a feeling of abdominal fullness or pressure that occurs shortly after a meal. Also known as post‑meal bloating, it often signals an imbalance in digestion.
Food intolerance, a non‑immune reaction to certain foods that can cause gas, cramps and swelling is one of the most common triggers. Lactose, gluten, and certain fermentable carbs (FODMAPs) sit high on the offender list. When your gut can’t break down these molecules, bacteria ferment them, releasing excess gas that swells the belly. Swapping out trouble foods or using an elimination diet often clears the fog fast.
Digestive enzymes, proteins that speed up the breakdown of fats, proteins and carbohydrates in the stomach and small intestine act like a backstage crew for smoother digestion. Taking a lactase supplement before dairy, or a broad‑spectrum enzyme mix with a heavy meal, can cut down the fermentable leftovers that fuel bloating. Most people notice relief within minutes, especially when the enzyme dose matches the meal size.
Irritable bowel syndrome (IBS), a functional gut disorder characterized by abdominal pain, irregular bowel movements and gas buildup often disguises itself as chronic post‑meal bloating. In IBS, the gut’s nerves overreact to normal stretch, sending pain signals even when the stomach is only mildly full. A low‑FODMAP diet, stress‑reduction techniques, and sometimes prescription medications help calm the gut’s over‑sensitivity.
Dietary fiber, the indigestible plant material that adds bulk to stool and feeds healthy gut bacteria can be a double‑edged sword. Soluble fiber (like oats and psyllium) absorbs water and forms a gel that slows digestion, often easing bloating. Insoluble fiber (like wheat bran) speeds transit but can add gas if introduced too quickly. Gradually increasing soluble fiber while staying hydrated usually smooths out the ride.
Beyond food, everyday habits play a big role. Eating too fast traps air in the stomach, while chewing gum or drinking carbonated drinks pours extra gas straight into the gut. Sitting upright after meals encourages gravity‑assisted gastric emptying; slouching or lying down can slow the process and let pressure build. Simple tweaks—slow bites, no straw, a short walk—cut the air‑in‑and‑out cycle.
Some medications also tip the balance toward bloating. NSAIDs, certain antibiotics, and even some antidepressants can alter gut motility or the microbiome, creating a perfect storm for gas. If you suspect a prescription is the culprit, talk to your doctor about timing, dosage changes, or alternatives before stopping anything on your own.
When bloating becomes persistent, severe, or paired with weight loss, vomiting, or blood, it’s time to get a professional look. Tests like a hydrogen breath test, stool analysis, or imaging can pinpoint lactose intolerance, bacterial overgrowth, or structural issues. Knowing the exact cause guides the right treatment, turning vague discomfort into a clear action plan.
Below you’ll find a curated set of articles that dive deeper into each of these angles—genetic factors, medication side‑effects, supplement comparisons, and more—so you can pick the tools that match your situation and start feeling lighter sooner.
Choosing the Best Diet to Prevent Bloating After Meals
Learn how to pick the right diet to stop post‑meal bloating. This guide covers low‑FODMAP, fiber, probiotics, portion control, and a practical seven‑day plan.
Read More