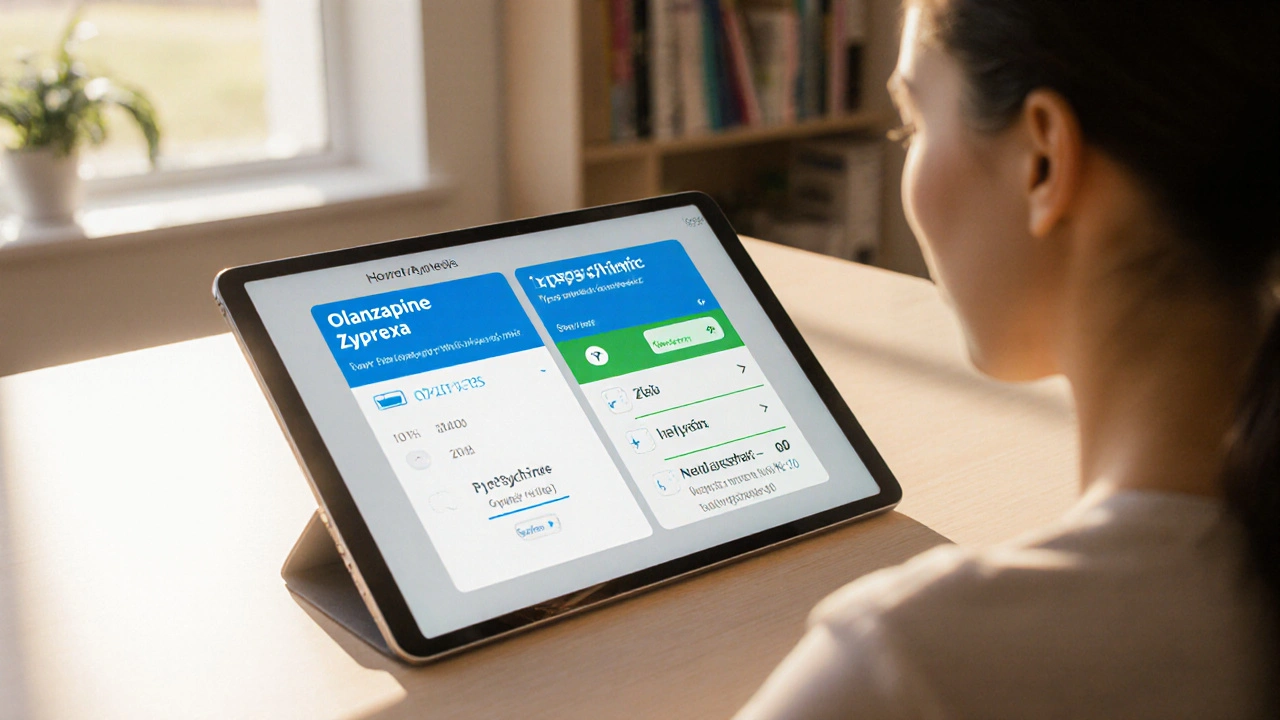
Antipsychotic Comparison Tool
Olanzapine (Zyprexa)
Typical Daily Dose: 5-20 mg
Weight-Gain Risk: High
Metabolic Impact: Significant (↑ glucose, lipids)
EPS Frequency: Low-Moderate
Special Monitoring: Baseline labs, periodic weight/BMI
Select Alternative
When a doctor prescribes Olanzapine for schizophrenia or bipolar disorder, patients often wonder if there’s a better fit-maybe a drug with fewer side effects or a simpler dosing schedule. This guide breaks down how Zyprexa (Olanzapine) stacks up against the most common alternatives, so you can talk with your clinician confidently.
Key Takeaways
- Zyprexa is highly effective for acute psychosis but carries a strong risk of weight gain and metabolic issues.
- Risperidone and Aripiprazole are popular first‑line choices when weight is a concern.
- Quetiapine offers sedation benefits for patients with insomnia but may cause low blood pressure.
- Clozapine remains the gold standard for treatment‑resistant schizophrenia, despite needing regular blood monitoring.
- Choosing the right drug depends on efficacy, side‑effect profile, dosing convenience, and personal health factors.
What Is Zyprexa (Olanzapine)?
Olanzapine is a second‑generation antipsychotic, also known as Zyprexa. It works by blocking dopamine D2 and serotonin 5‑HT2A receptors, helping to calm hallucinations and mood swings. First approved by the FDA in 1996, Olanzapine is available in tablets, orally disintegrating tablets, and a long‑acting injectable form.
How Olanzapine Works
The drug’s dual dopamine‑serotonin blockade reduces the overstimulation that leads to psychotic symptoms. By moderating these pathways, patients often see rapid improvement in thought disorder, delusions, and manic episodes. However, the same receptor activity also influences appetite regulation, which explains the notorious weight‑gain side effect.
Primary Uses
Olanzapine is FDA‑approved for:
- Schizophrenia
- Bipolar I disorder (manic or mixed episodes)
- Maintenance treatment of bipolar disorder
- Adjunct therapy for major depressive disorder (when combined with fluoxetine)

Side‑Effect Profile
While many patients tolerate Olanzapine well, clinicians keep a close eye on:
- Weight gain: Average increase of 4‑10kg in the first six months.
- Metabolic syndrome: elevated fasting glucose and triglycerides.
- Sedation and drowsiness, especially at higher doses.
- Extrapyramidal symptoms (EPS) are less common than with older antipsychotics but can still occur.
- Elevated prolactin levels in some individuals.
Top Alternatives to Olanzapine
Below are the most frequently considered substitutes, each marked up for easy knowledge‑graph extraction.
Risperidone
Risperidone is a second‑generation antipsychotic that offers strong dopamine blockade with a lower propensity for weight gain. Typical starting dose is 1mg daily, titrated to 4‑6mg for schizophrenia. It’s praised for its relatively flat metabolic profile, though it can cause higher rates of EPS at doses above 6mg.
Quetiapine
Quetiapine (Seroquel) is known for its sedating effect, making it useful when insomnia co‑occurs with psychosis. Doses range from 150‑800mg daily. While weight gain is moderate, orthostatic hypotension can be an issue, especially when standing up quickly.
Aripiprazole
Aripiprazole works as a dopamine partial agonist, which often translates to less sedation and minimal weight gain. Starting at 10‑15mg daily, it can be increased to 30mg. Some patients report activation (feeling jittery), but metabolic side effects are among the lowest in its class.
Clozapine
Clozapine is reserved for treatment‑resistant schizophrenia because of its superior efficacy. Doses begin at 12.5mg twice daily, targeting 300‑600mg. The trade‑off is a mandatory weekly blood test to monitor for agranulocytosis, plus a higher risk of seizures and myocarditis.
Haloperidol
Haloperidol is a first‑generation (typical) antipsychotic, valued for its potent dopamine D2 antagonism. It’s often used in acute agitation at doses of 5‑20mg daily. Weight gain is minimal, but EPS and tardive dyskinesia are common concerns.
Side‑by‑Side Comparison
| Drug | Typical Daily Dose | Weight‑Gain Risk | Metabolic Impact | EPS Frequency | Special Monitoring |
|---|---|---|---|---|---|
| Olanzapine | 5‑20mg | High | Significant (↑ glucose, lipids) | Low‑Moderate | Baseline labs, periodic weight/BMI |
| Risperidone | 1‑6mg | Low‑Moderate | Modest | Moderate (dose‑dependent) | Prolactin if >6mg |
| Quetiapine | 150‑800mg | Moderate | Moderate | Low | Monitor blood pressure |
| Aripiprazole | 10‑30mg | Low | Minimal | Low | Watch for activation |
| Clozapine | 300‑600mg | Moderate‑High | High (requires fasting glucose) | Low | Weekly ANC counts |
| Haloperidol | 5‑20mg | Low | Minimal | High (tremor, rigidity) | EPS rating scales |
How to Choose the Right Antipsychotic
Think of medication selection as a balancing act between three main factors:
- Efficacy for your specific symptoms. Some drugs calm agitation faster; others excel at preventing relapse.
- Side‑effect tolerance. If you’re already managing diabetes, a drug with low metabolic impact (like Aripiprazole) may be wiser.
- Practical considerations. Daily pill versus long‑acting injection, need for blood tests, cost, and insurance coverage all play a role.
Discuss each point with your psychiatrist. Bring a list of any existing health conditions, current meds, and lifestyle factors. That way, the clinician can match the drug profile to your personal context.
Frequently Asked Questions
Can I switch from Olanzapine to another antipsychotic safely?
Yes, but the transition should be supervised. Doctors usually taper Olanzapine while introducing the new drug to avoid withdrawal or symptom rebound. A cross‑taper over two to three weeks is common.
Why does Olanzapine cause so much weight gain?
Olanzapine blocks histamine H1 receptors and serotonin 5‑HT2C receptors, both of which regulate appetite. The blockage increases hunger and reduces satiety, leading to calorie over‑consumption.
Is the long‑acting injectable form of Olanzapine better than the oral tablet?
Injectable Olanzapine (every 2‑4 weeks) can improve adherence for patients who miss daily doses. However, it shares the same side‑effect profile, and injection site reactions can occur.
What should I monitor while taking Olanzapine?
Track weight, fasting glucose, lipid panel, and blood pressure every 3‑6 months. Report any sudden drowsiness, muscle stiffness, or unusual mood changes to your provider.
Are there any non‑pharmacological options that work with these meds?
Cognitive‑behavioral therapy, family education, and regular exercise can boost medication effectiveness and help manage side effects like weight gain.
Next Steps
If you’re currently on Olanzapine and uneasy about side effects, start by scheduling a medication review. Bring recent lab results, a list of all prescriptions, and any concerns about weight or energy levels. Your psychiatrist can then propose a tailored switch-perhaps to Aripiprazole for metabolic safety or to Clozapine if symptoms remain uncontrolled.
Remember, no single drug works for everyone. The best choice balances symptom control with quality of life. Armed with this comparison, you can have a clearer conversation and move toward a treatment plan that feels right for you.

Post A Comment