Understanding Benign Prostatic Hyperplasia (BPH) and Kidney Health
As we grow older, our bodies undergo various changes that can impact our overall health. One such change is the enlargement of the prostate gland in men, a condition known as benign prostatic hyperplasia (BPH). In this article, we will explore the relationship between BPH symptoms and kidney health, providing valuable information on how to manage and prevent complications.
To better understand this relationship, let's first take a look at what BPH is, how it affects the urinary system, and its potential impact on kidney function.
What is BPH and How Does it Affect the Urinary System?
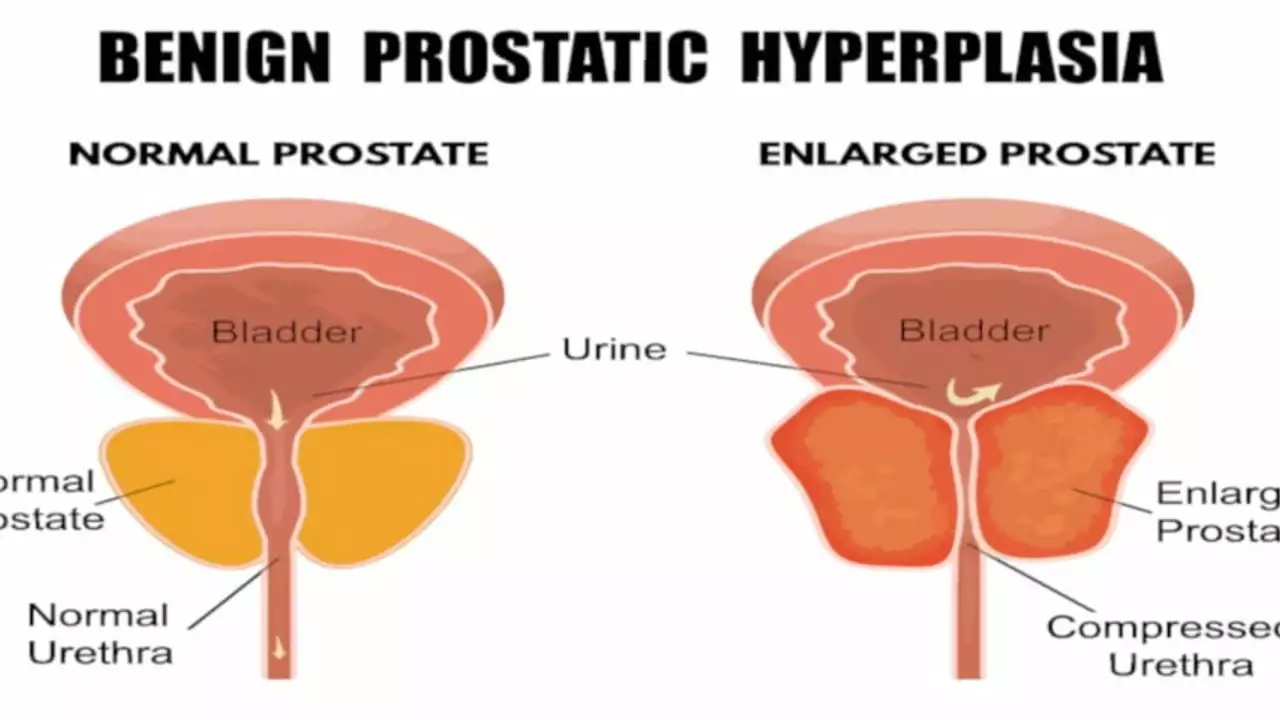
Benign prostatic hyperplasia (BPH) is a noncancerous enlargement of the prostate gland, which is responsible for producing the fluid that nourishes and transports sperm. As the prostate enlarges, it can compress the urethra, leading to difficulties in urination.
The urinary system consists of the kidneys, ureters, bladder, and urethra. The kidneys filter waste and excess fluids from the blood and produce urine, which travels down the ureters to the bladder. The bladder stores urine until it is released through the urethra during urination. When the prostate enlarges and compresses the urethra, it can obstruct the flow of urine, leading to a range of symptoms and potential complications.
Common BPH Symptoms and Their Impact on Kidney Health
BPH symptoms can vary in severity and often worsen over time. Some common symptoms include frequent urination, a weak or interrupted urine stream, difficulty starting or stopping urination, and the sensation of incomplete bladder emptying. These symptoms can be uncomfortable and disruptive to daily life, but they can also lead to more serious complications if left untreated.
When the flow of urine is obstructed, it can cause a buildup of pressure in the bladder and kidneys. Over time, this increased pressure can damage the delicate filtering structures within the kidneys, potentially leading to chronic kidney disease or kidney failure.
Diagnosing BPH and Assessing Kidney Function
If you are experiencing symptoms of BPH, it is important to consult with a healthcare professional for a proper diagnosis and assessment of your kidney function. This may involve a physical examination, a review of your medical history, and various tests such as blood tests, urine tests, and imaging studies.
Your healthcare provider may also recommend more specialized tests to evaluate the severity of your BPH symptoms and their impact on your kidney function. These tests may include a prostate-specific antigen (PSA) test, a urodynamic study, or a cystoscopy.
Treatment Options for BPH and Protecting Kidney Health
There are several treatment options available for BPH, ranging from lifestyle changes and medications to minimally invasive procedures and surgery. The choice of treatment will depend on the severity of your symptoms, your overall health, and the degree of impact on your kidney function.
Lifestyle changes, such as reducing fluid intake before bedtime, avoiding caffeine and alcohol, and practicing double voiding, can help alleviate some BPH symptoms. Medications, such as alpha-blockers and 5-alpha-reductase inhibitors, can help relax the prostate and shrink its size, respectively, improving urine flow and protecting kidney function.
Minimally Invasive Procedures for BPH
If lifestyle changes and medications are not effective in relieving your BPH symptoms, your healthcare provider may recommend minimally invasive procedures. These procedures typically involve the use of heat, laser, or other energy sources to remove or destroy prostate tissue, thereby relieving pressure on the urethra and improving urine flow.
Some examples of minimally invasive procedures for BPH include transurethral microwave thermotherapy (TUMT), transurethral needle ablation (TUNA), and laser therapy. These procedures are generally less invasive than surgery, have a lower risk of complications, and can help protect kidney function by improving urine flow.
Surgical Options for BPH
In more severe cases of BPH, or when other treatment options have failed, surgery may be recommended. The most common surgical procedure for BPH is transurethral resection of the prostate (TURP), which involves the removal of a portion of the prostate gland to relieve pressure on the urethra and improve urine flow.
Other surgical options include open prostatectomy, which involves the removal of the entire prostate gland, and minimally invasive surgeries such as laparoscopic prostatectomy and robotic-assisted prostatectomy. These surgical options can effectively treat BPH symptoms, but they may carry a higher risk of complications and a longer recovery time.
Preventing BPH-Related Kidney Damage
Early detection and treatment of BPH are crucial to preventing kidney damage and maintaining overall kidney health. Regular check-ups and screenings, especially for men over the age of 50, can help identify BPH early and allow for prompt intervention.
Maintaining a healthy lifestyle, including staying physically active, eating a balanced diet, and managing stress, can also contribute to better prostate and kidney health. If you are concerned about your prostate or kidney health, consult with your healthcare provider to discuss the best course of action for your specific situation.
Conclusion: The Importance of Addressing BPH Symptoms and Kidney Health
In conclusion, BPH symptoms can have a significant impact on kidney health if left untreated. Understanding the relationship between these two conditions, recognizing the symptoms of BPH, and seeking prompt medical intervention are crucial to preserving kidney function and overall well-being.
By staying informed about BPH and kidney health, you can take an active role in managing your symptoms and preventing complications, ensuring a better quality of life in the long term.

Post A Comment